- Home
- keyboard_arrow_right Phelan Dental Seminars
- keyboard_arrow_right How do you treat a non-restorable central incisor in your practice?
How do you treat a non-restorable central incisor in your practice?
Dr. Jim Janakievski August 30, 2011

How do you treat a non-restorable central incisor in your practice?
If an implant is to be placed, should we perform the procedure as an immediate extraction socket placement or should we delay the implant placement?
I am sure we have all had a patient like this walk into our practice. The patient has a history of trauma at a young age with subsequent endodontic therapy. Years of loading further weaken the tooth. Her dog recently bumped her in the mouth and now she feels that her tooth is loose. You determine that the crown is fractured and the tooth has a poor restorative prognosis.
How do you plan this treatment with your team? Should the surgeon place an immediate implant at the time of extraction?
To determine the most predictable treatment option, we must take into consideration the shape and dimensions of the labial bone, the existing soft tissue profile and the amount of apical bone available for implant stability.
From the clinical exam, we can determine that the soft tissue profile of the hopeless incisor is similar to the adjacent central. When considering immediate implants or simultaneous procedures, I always prefer to have a favourable soft tissue position prior to surgery. The slight crestal bone remodeling after the extraction will lead to reduced support for the gingiva with resulting recession. So we either have a gingival level that is coronal to ideal, or our procedure must provide some additional support or augmentation.
Next we can look at the radiograph to evaluate the interproximal and apical bone. For this patient, we note that the bone appears to be at a normal level on the mesial and distal of the root and adjacent teeth. The apical bone is without a lesion and it is sufficient for implant anchorage.
Lastly, we will need to evaluate the facial bone. This can be done with a CBCT or clinically at the time of surgery. Insufficient labial bone can be a risk when attempting to place an immediate implant. It is best to stage the procedure with alveolar ridge augmentation and a delayed implant placement. For this patient, the labial bone had both a normal crestal level and facial thickness.
The implant was placed immediately at the time of the extraction for this patient. In the next blog posting, we will look at how I managed the soft tissue form.
Full Smile View
Retracted View
Crown Fracture Resulting In Inadequate Tooth Structure For Predictable Restoration
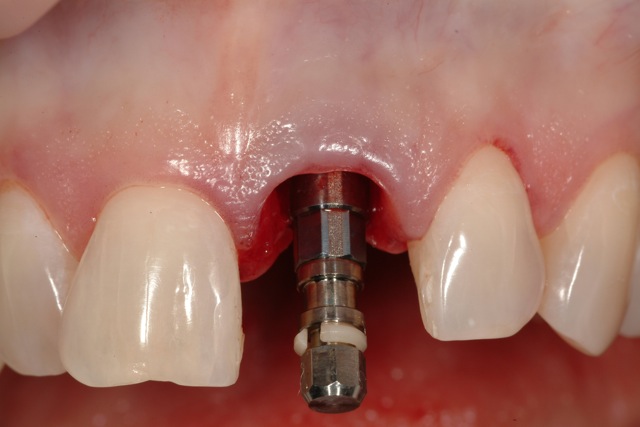
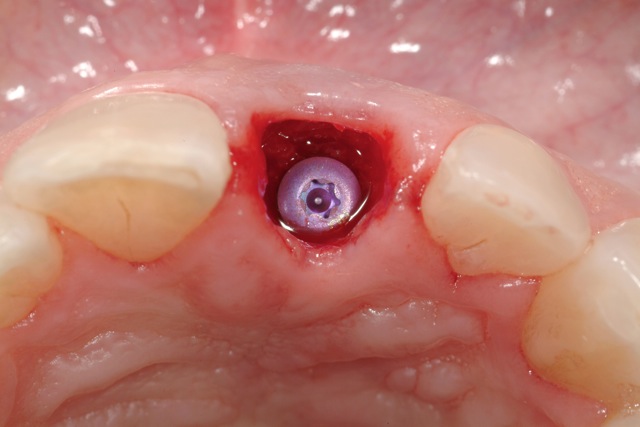
Dental Implant Placed With Platform 3 mm Below The Free Gingival Margin
Dental Implant Placed Towards Palatal Aspect Of Socket With Bone Augmentation In Residual Socket
Radiographic Evidence Of Large Pulpal Chamber And Extent Of Fracture Line. There Is Abscence Of Any Peri-Radicular Lesion.

Post comments (1)
© Copyright Phelan Dental Seminars I Dr. Stephen Phelan






Lea Kozubal on October 26, 2015
Hey, I am considering undergoing breast augmentation surgery. My problem is about going under muscle as I’m very active meaning that I do crossfit. Does anyone have any feedback? I am still to see the the doctor as I am still not quite ready for the procedure. Thanks