- Home
- keyboard_arrow_right Phelan Dental Seminars
- keyboard_arrow_right Would you extract this tooth or not?

I wanted to share with you a case that presented to my office a few months ago and see what your opinion would be about the best approach for treatment.
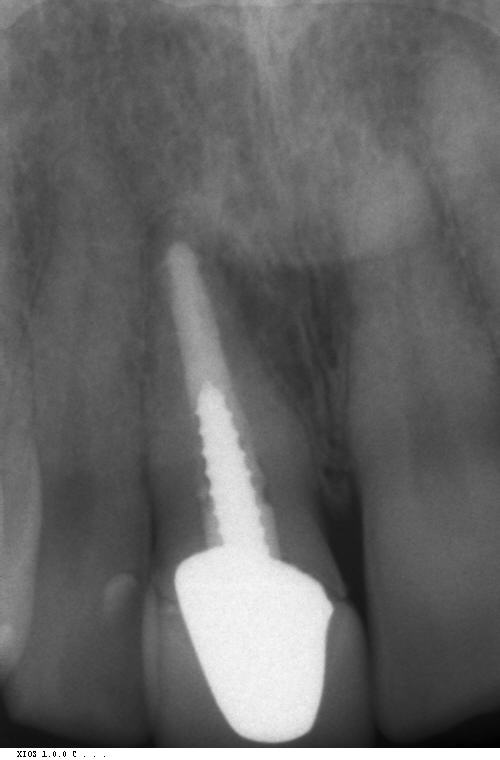
With this case the patient presented with a central incisor that had previously been treated with an endo, post, core build-up and crown. The problem was that something was loose. In this particular case the margins were not supragingival so it was hard to tell what exactly was loose!
In a case like this, either the entire tooth, post core and crown is loose or the post core and crown is loose, or maybe just the crown is loose.
I really could not tell during the emergency visit so I decided to reappoint the patient a few days later when I had more time to assess the situation and provide some form of treatment.
At the next appointment I tried to remove the crown and the post, core, and crown came out in one piece. You can see by the photo that there is not very much remaining tooth structure and minimal ferrule. The remaining root has a small amount of recurrent decay but no mobility and normal periodontal architecture.
I provided the patient the following options for treatment:
- Remove the remaining root, graft and place an immediate implant.
- Remove the remaining root, graft the socket and plan to place an implant 3 months later.
- Remove the remaining root, graft the socket and prepare the adjacent teeth for a fixed bridge
- Remove the remaining root and prepare the adjacent teeth for a fixed bridge without grafting the socket
- Remove the remaining root and place an RPD.
- Recement the post, core, and crown
- Crown lengthening surgery followed by a new post, core and crown
As you can imagine giving the patient a list of options like this is important for informed consent but can lead to confusion for the patient to make a decision.
In a case like this the patient will inevitable ask you what you would recommend for the treatment if this were your tooth.
What I would like to know is how you would treat this patient. I gave the patient 7 options for treatment and I would like to find out your treatment recommendation if this was your patient. You can leave your treatment choice and comments using the link above this post.
Next week I will share with you the treatment the patient has received for this case.
Post comments (184)
© Copyright Phelan Dental Seminars I Dr. Stephen Phelan






PPM Software on June 25, 2024
Thank you so much for sharing the fantastic tips. I loved it!
Navya on June 24, 2024
Lovely Post. Thanks for sharing it!
Daisy C. See on May 25, 2021
The work I would do might be the last treatment the tooth can receive. It is at the situation at not very much remaining tooth structure, minimal ferrule and it also noted, the remaining root has a small amount of recurrent decay but no mobility and normal periodontal architecture. Radiographically, the root length is not symmetrical with the adjacent incisor, slight extrusion and happened. There is also a break in the lamina dura at the apical third of root portion, somewhat radioluscency can be seen, though no pain was mentioned, maybe negative to percussion (asymptomatic). My treatment will depend on the eagerness of the patient to keep it and the budget the patient has. I will try to explain everything with the patient that longevity is not guaranteed. I will still give the patient 2 remaining option for him to decide:
1. After crown lengthening, add ferrule then I will put FiberSite Post produced by Megadental Italia and then put a no contact non- metal crown. 2. Remove the remaining root, graft the socket and place RPD and plan to place an implant 6-8 months later for full recovery.
Eftekhar Arshadi on April 21, 2021
Hello Dr Phelan
An ordinary and every day case. Good educational case for us. Thank you for sharing it. It seems to me the pt is a grinder and the crown has a tight contact with # 25,26 this culd be the reason for lose crown. It needs probing to check biological width and the reason for black mark on BuccaL. I would give the pt the following treatment plan.
1- check the endo
2- crown crown lengthening
3- post and core # 8 with all ceramic crown
4- porcelain venners # 6,7, 9,10,11 and lower from 22-27 correcting anterior bite and guiadance.
Vladimir Dincic on January 30, 2021
Hi everyone, I believe that we have to try to save any tooth that has good periodontal architecture, with no fractures of the root, so the option number 7 would be my choice with crown lenghtening surgery followed by new post, core and crown but first i would do endo retreatment because of the protocole that any endo treatment that is older than 6 months should be retreated
Albana on January 18, 2021
Good done but i would prefer a little gingivectomy before.to reshape dhe aspect of vestibular margin.the rest,super.
Mandla Simelane on January 8, 2021
Assuming intact apical/ periapical integrity and no root fracture, and patient had asked me what will I do, I will give the patient the following options and base them on the longevity, conservation, and the predictability of the outcome;
1. Crown lengthening and provision of a post crown – Warn patient that since a lot of work has been done on the tooth / remaining tooth structure , this treatment may come under due stress and fail prematurely.
2. Extraction/ socket grafting / preservation and provision of an implant either immediate or 3 months later
Babak Teshfam on November 28, 2020
In my humble opinion our treatment depend on some measurement like how much of tooth structure will be remaining after removing the infected dentin.how long the tooth will be top prepare after having at least 2mm ferrule structure and a definite finish line. If everything meet my standards of treatment I will go with crown lengthening followed by post and core and crown.But otherwise I will go with placement of implant which the options that you gave to the patient depends on the collusion type of person, oral hygiene , medical history.If it was nothing to be worried about I will choose an Extraction and immediate implant placement following a graft placement.
Loudine Van Wyk on August 5, 2020
I will try new core and post, with the core and post cemented as a single, bonded unit. I like fiber Site post which transfer the forces into the base of the core for compromised roots.
Loudine on August 5, 2020
I will try new core and post, with the core and post cemented as a single, bonded unit. I like fiber Site post which transfer the forces into the base of the core for compromised roots.
Khawla aboudiab on August 5, 2020
Hi Dr,
I would go with crown lengthening , fiber post , 2-3 pins , build up and new crown.
Helene on May 31, 2020
Depends the age of the patient and the age of the post and core and crown. Ideal would be to extract if there was enough maxillary bone to support an implant but if time was an issue( or age) I would recement the existing P&C and crown. Not sure what the post was made of so may consider new post & core with glass resin posts if the recementing should fail soon Also, not sure why it was loose to begin with, trauma? time?
Diana Muzic on May 21, 2020
I will recement post, core and crown.
DR MD TARIQUZZAMAN on May 18, 2020
Hello Dr
I would go for extraction and followed by immediate implant with GBR.
John Epperson on April 6, 2020
Needed: 3-D scan showing buccal bone thickness.
At the time of extraction, If the root can be removed atraumatically and the socket is healthy, with no loss of buccal bone, then place an immediate implant, use clear plastic retainer with a cosmetic tooth #8. Restore after integration. Otherwise , extract, graft, implant after healing.
Long term replacement.
Ted Margel on March 28, 2020
Depending on the patients age (appears relatively younger) and expectations, I would favour the immediate extraction with grafting and provisional. IMO, a new post, core crown will only give you another 5-10 years of service.
Dominique on March 22, 2020
Give all above options (with the exception of #6, patient would return in a couple of days, disrupting their schedule and yours) with the understanding that the prognosis is undetermined.
However, in my 27 years of experience, I believe that those options would yield a less than ideal long-term result. If it were my tooth, I’d extract, graft, place an implant in 3 months… all due to “the rule of ferrule”, continued trauma to the bone, better esthetics and tissue health, time, finances and longevity.
However, I’m just a Dental Assistant.
Ross on March 18, 2020
All of the above plus Option 8: non-metallic post with “composite resin crown” + – crown lengthening
Lana on March 9, 2020
I think I will preserve with crown lengthening and fiber post &build up
Then crown , I don’t like metal posts any more
But we have to till the patient that the prognosis is questionable because we don’t have enough ferrule
Navneet Rai on February 29, 2020
Extraction,Gbr if buccal wall is missing. Place implant,since looks like a guarded prognosis
Mansi Ghanshani on February 14, 2020
Hello Doc,
I would do crown lenghthening followed by custom post & core & crown for the above patient.
Ivan Ho on November 3, 2019
Option 1
Rumisa on January 8, 2020
Hi Dr
love the clarity of ur cases
I would surely go with the same treatment but additionally I would also do small amount of crown lengthening as I could see that there is a provision for that in gumline.
For me priority is to save what is natural.
Evelyn Estefan on July 30, 2020
Hello Dr. Phelan,
Seeing the above X-ray, I would take the conservative approach to re-cement , nonetheless give patient all options.
Have them Sign consent of risk of failure and possible outcomes.
Should they request recement Option, then
Take EOC pictures
Intraoral 3 D image, I use Cerec
PA X-ray and Pano
Perform ADA
D4211 1 tooth
D2954 Post Core
D2920 Recement crown
Sigh treatment Plan as well.
Anesthesia, Light electrogingivectomy with ultra fine tip to expose outermost margin.
Try in crown fit at margin If all good then proceed to
Clean canal then irrigate with Endo irrigators Hypochlorite
remove snare layer with EDTA dual then CHX 2%
Check for root caries If all clear place non metallic post cemented with infinity or such
Make core build with core paste white from Denmat Try in crown again Check for Inter proximal contact point tightness With a floss marked with articulating paper, recement crown with very light functional Occlusion and check for early contacts and equilibrate,recomend a functional protective guard if needed.
Thank you.
Evelyn Estefan, DDS
Anita on August 28, 2020
I would try to find out the cause of failure for this post restoration like any premature contact or high points and go for new post restoration.
Gladys on November 3, 2019
Options 2
Thanks
sushmitha Jeeri on July 1, 2019
Hey Dr. phelan, I would do option one or save the tooth depending on the finances. But I would inform the patient that prognosis is fair to poor. I have a question do we discuss with the patient about the grey area?
Noha on June 1, 2019
Thanks for sharing Dr Phelan. I have no experience in Implants however I am learning about them. Assuming patient is medically fit and the bite isn’t with interferences, and depending to finances I would go with option 1 or 2. Thanks
Peter Smyth on March 3, 2019
Good job.
If the patient is not concerned with aesthetics of the grey root showing through then keep the tooth as it appears there is enough root structure to ferrule, however, I would get a CBVT. Assess the root proximity to the lateral and any fractures. It’s likely there was movement as the screw post was into the GP. Bonded gold post and core with new PFM would be quite adequate. Otherwise remove root. Graft and delay implant placement.
Gladys on November 3, 2019
Options 2
Thanks
Idrees on March 1, 2019
Option 7 I think it’s a metal post so replace with fiber post
Mandla Simelane on February 10, 2019
It will depend on risk assessment and cost factors- Put it differently- on Bio-Psycho-Socio-Economic status of the patient.
Angela Lowe-Ho on May 2, 2019
Another option is to clean out the post space, irrigate sodium Hypochlorite 4%, EDTA, bond ribbond in post space, extend the ribbond
also to be a core, doubled up and build a composite crown so long as you get the occlusion free and create enough space. This option would be helpful for a patient with limited finances and not wanting a removable partal denture. The dark neck area would need to be opaqued out.
Dhouha s toma on November 26, 2018
Hello dr Stephen
Though iam not officially a dentist till now
But i think we have to extract it then we do an implant
Thanx for sharing this case
Dr hafsa al idrissi on October 27, 2018
I would explain both long term prognosis and short term, providing the options of saving the tooth by placing post core and crown or extracting the tooth , socket preservation, provisional removable prosthesis (6-8) and after than place an implant with a screw retained provisional ( make sure it’s off loaded) . Wait for the healing period and contour the Pontic area every 3 weeks to shape the emergence profile of the tooth implant supported in the future. And finally when implant is osseointegrated take impressions for the crown.
Theingi on September 8, 2018
I will remove the caries and recement the new post, core and crown. The gingival height is quite the same as adjacent tooth so I won’t do the crown leangthening procedure if I can completely remove the caries.
Margarita Aleksanyan, DDS, AAACD on May 1, 2018
I agree with Dr. Ferres. There are also couple other considerations – gingival height of #8 is more coronal than #9. Pt. also has a thick gingival architecture which is great. Some gingival recession after immediate implant placement and provisionalization will happen. Most likely we can achieve the same gingival height on #8 as it is on #9. If that’s not the case, pt. has gingival recession on the left side and if necessary slight crown lengthening can happen on the right side.
One new method that Dr. Salama was describing in his recent presentation was partial root extraction. With this method very thin (1 mm of buccal root portion) is remained in the socket and it actually preserves the buccal bone and gingival recession. Not very many surgeons are currently implementing that technique though.
pooja on February 14, 2018
Hello
I would suggest for option 2 if patient is ready for implant and a treatment plan which has best success rate.
Option 7 has very little rate for getting best result as there is very less tooth structure left and part of it has caries .so after cleaning out the decayed part I feel to reatian a post is challenging and also needs crown lengthening which will disturb gingival contour with adjacent teeth.
Dr.shubana on December 23, 2017
cleaning the caries then option 7
H on November 22, 2017
I would assess if there is a vertical root fracture . If not, crown lengthening can be achieved by removing soft tissue only and not bone it seems from the X-ray., preserving the 1:1 crown root ratio. I would inform the patient of the unpredictability of option 7, if they opt for it, it could be tried , I would say Grafting and implant 3 months later is more predictable though.
Dr kavita on November 22, 2017
The treatment depends on the patient’s general health , age factor, and willing for surgery or not and mainly cost. Keep all this factor we can take decition and if try to save the patient natural remaining root / tooth structure we can save and do the needfull, if patient ask anything about asurity of the treatment for any 10% failure case we have to think about patient convenient treatment.
Anisa on October 28, 2017
Crown lengthening surgery followed by a new post, core and crown ,
fariha khan on October 8, 2017
will go with option 7
fariha khan on October 8, 2017
as you have already mentioned that the tooth is not mobile with normal PDL and little recurrent caries so i would go with option 7 crown lengthning and then new post core and crown.
fariha khan on October 8, 2017
as you have already mentioned that the tooth is not mobile with normal PDL and little recurrent caries so i would go with option 7 crown lengthning and then new post core and crown
Clara Iwuoha on October 4, 2017
From the assessment you gave; The root is not mobile and has normal periodontal architecture, I will opt for option 7,that is,Crown lengthening surgery followed by a new post ,core and crown.Thanks for sharing your experience with me
luis marroquin on September 18, 2017
Dear
Thanks for sharing these cases with us
3 options:-
1 extrusion, new casted post and core, and crown
2 .7
3, implant
Imad rekab on September 10, 2017
Hello Dr. Stephen
What you should do if it is your tooth
May be if I am the patient , I will go for the first option to rebuild the tooth
with post and core and a crown, and I’ll keep in mind the treatment may not
last long . But I’ll give the tooth a chance .
But the question is ? Not all patients understand this option if the treatment fails.
So he will come to the clinic carrying his crown and he will tell you this is your treatment
So I’ll prefer to go for grafting the socket and immediate implant placement to be on the safe side .
lone Snedker on August 7, 2017
The X ray does not show endo problems as such, so why reendo? The only reason is exposure because of the lost crown. Is there an infraction? Due to a metal screw? If the patient is not concerned about the difference in gingival level, why no make a new post and a titanium crown? And make clear that later an implant can be necessary. But make sure there is no infraction
Mariel Nanut on June 29, 2017
Not option 1 :it’s a very wide root and near 12. Not a bridge . Not a RPD. I would recement with temporary cement and re endo.Wait some weeks.If it’s ok : option 7 and rh incisal 13 12 21 22 23 with composite or porcelain veneers (ay least 21 with porcelain veneer :it is better for the esthetic.Thank you !!!!!
Doris Ferres on June 28, 2017
Case to be handled with a very good plan. The number one priority is the preservation of the existing gingival architecture which looks great at this time. First: with a: CBCT, determine existing bone, If bone allows, atraumatic extraction and immediate implant placement, that would be the way to go since it would be the best to preserve the esthetics. 2. Wax up model to be used merging the CBCT with it to create a surgical guide for implant placement in the correct spot. Consider placing implant closer to the palatal wall and bone graft as needed to preserve bucal bone Remembering the 2mm rule surrounding implant for the prevention of bone loss. Also placing implant 3 mm from desired final gingival margin level will render a great result. And finally: a good screw retained temporary.
Sumaiya on June 28, 2017
I would go for option 6 or 7, depending which one has less disadvantages
Sean Harris on June 28, 2017
Option 6
I have this very same problem with my own tooth! Minus the decay. I don’t want a bridge or denture. If the root ever fractures I will go for implant. I brux and at present the tooth is on a fibre post. Last time it came loose the direct core actually deboned from the post. Some dodgy dentist in Florida stuck it back with a think cement. It didn’t fit. He ground the heck out of it. It’s still there 2 years on!!!
Adil Majid on June 27, 2017
Could you do a Richmond crown with a beveled margin to gain increased ferrule/retention, while dropping the margin slightly? It seemed like there was a little room to prep further sub-g and not violate biological width on the radiograph
Aya on June 27, 2017
Option #7
Dr Teresa DeStefano on June 27, 2017
Wax up/ surgical guide/ Scan- then decide if immediate ext/ implant placement/ immed provisional ( screwed in) is feasible.
Alexander Swinkels on June 12, 2017
The gumline of 11 is lower than that of 21. There are No apical inflamtions or anything so my choice would be crownlenghtening, endo- revision, post/core and a New crown. The best implant is still No implant.
FOUAD MEDOUAR on May 25, 2017
Dear Dr Stephen.
Sorry for my english I’m francophone. I saw your video and I want to thank you for sharing it with us it’s really helpful. I think it depends firstly of the finances of a person. The best solution would be solution 2. But I learned at the University of Paris 6 that the best implant was our root. The disadvantage is the blackness of the root which can be solved by an zyrconia inlay core and a non-metal restoration (ceramic). The problem is high rate of fracture for porcelain-veneered zirconia-based restorations that varies between 6% and 15% over a 3- to 5-year period, while for ceramo-metallic restorations the fracture rate ranges between 4 and 10% over ten years ( Zirconia in fixed prosthesis. A literature review (Rubén Agustín-Panadero, Juan L. Román-Rodríguez, […], and Antonio Fons-Font)
For this reason, I prefer the solution 1 and 2.
Dr Fouad Medouar
Aimn Abbasi on May 24, 2017
Hi,
If the caries is not soft and arrested, option #6 and re-eval to start off with; Option #7 is a viable option but the black triangle might arise as an issue with less inter dental papilla fill, which again depends on the crestal bone height and contact point, Option #1 looks feasable since esthetic zone and if #6 does not work successfully,
One option not mentioned could be Decoronation with bridge.
Thanks,
Steven Foxn DDS, FACD on May 22, 2017
Since we do not have information on the patients occlusion, parafunction, vertical and horizontal overlap, no clinical exam or articulated diagnostic casts, we are limited.
We all know the problems of this type of care. One item we forget about is the elastic modulus of the tooth. If I remember back to dental school, the elastic modulus is a value used to measure the rigidity of the teeth. For human teeth, indicates the ability of enamel and dentin to resist elastic deformation.
As the tooth looses enamel/dentin, its ability to resit elastic deformation decreases, the tooth becomes more “flexible”. As the tooth becomes more flexible, it may reach a level which breaks the cement bond, leading to recurrent caries and/or loss of restoration.
We have all restored teeth with extensive tooth loss which have suffered from loss of restoration or recurrent caries. Now there is a responsibly of the patient with home care which is also an important factor said.
Clinical studies with teeth restored endodontics, post and and crown, show similar longevity as single implants. But the tooth in the example has most if not all the enamel and dentin removed, compromising restorability.
If we do opt for post/core buildup and appropriate crown, we most certainly must have crown lengthen. Can periodontist provide enough for an adequate ferrule? AND, the crown lengthening will change the gingival architecture, and the anterior esthetics.
With all that said, I would opt for extraction and Implan
Marwa on May 22, 2017
Option7
Marwa on May 22, 2017
Option 7
Dr. TALAL on May 21, 2017
I would go for the following option,
Remove the remaining root, graft the socket and plan to place an implant 3 months later.
Raza siddique on May 21, 2017
I will go with option 1 .
Zartaj on May 20, 2017
Extraction followed by grafting and immediate implant is my choice!
Zartaj on May 20, 2017
Extraction followed by grafting and immediate implant.
DrSubasinghe on May 19, 2017
Seems like there is a fracture and some inflammation in the buccal region. In this scenario, I would remove the root very carefully, then leave it for 6-8 weeks with one course of antibiotics starting 1 hour prior to extraction.
Thanks will take a CT and plan the treatment. Will provide temporary solution via palatal implant, stick truck, partial!
Cheers
J
Thank you Dr.Phelan
Dr Nagarathna PJ on May 18, 2017
I would like to go with the last option but doubtful about the retention at core?even after crown lengthening. In that case option 1 is better
mydentalcareguide.com on May 8, 2017
Before your dentist can even consider pulling your tooth, certain steps must first be taken. Doing so not only helps to insure that your extraction will go as safely and uneventfully as possible but also that your tooth was removed for good reason.
Maitri on March 30, 2017
Patient will be very concerned about loosing his front tooth but decisions would depend on expectations, time frame ,how cosmetically inclined the patient is and of course finances.
Looking at the photos , left central and lateral have higher gingival margins compared to right central and lateral.
Hence crown lengthening will be a good option . Lasers could be used to contour right lateral as well.
There is wear of Incisal surfaces of all incisors – veneers with adjacent teeth would look good!!!
A. O. H. A on November 2, 2019
I will extract remaining tooth, graft and place implant in 3months.
Another option will be to extract and prepare the adjacent tooth for a fixed bridge.
Meenu on March 29, 2017
1. Extraction followed by grafting and immediate implant.
srikanth aluru on March 20, 2017
Consider extraction grafting and immediate implant placement, provided a satisfactory primary stability is achievable.
Ashish on March 16, 2017
I would like to opt for option 5 followed by option 2
Johann E. on February 10, 2017
Hi there,
Thanks for sharing this challenging case that can come to every dentist in a daily consultation.
Of course checking med history is mandatory.
Depends also on your own ability and the financial possibilities of patient. Does the blue-ish aspect of gingiva bother the patient?
I would not advice patient to remain as it is but would still re-cement on the day of assessment to allow for time to reflect on the part of the patient.
I would recommend later immediate placement of an implant with bone grafting and handling of the gingiva in the different stages following. The question is: what would patient gain from a delayed approach with grafting? If infection is what motivates you to delay, It is not absolutely the case here from what I can see.
Seeing so much decay on the remaining root means I would not advice for redoing endo + new post & core.
It would be impossible for me to promote a fixed bridge in this situation even though preps could be envisioned to put veneers on other teeth if occlusion allows and further evaluation shows it to be necessary.
Good luck in taking care of this patient!
Jakob Lempert on January 24, 2017
Good temporery cemention. Check carefully occlusion and articulation, dont forget protrusion. Follow symptoms. If everything seems ok then follow option 7. If symptomer that could be endo-like, then re endo. Otherwise go to option 2
But With 6-8weeks of healing before implant. Implants are ment to replace MISSING teeth not teeth that can be treated otherways
Kurt Marler on December 6, 2016
Depending on age and med history , and how much gingiva shows when smiling are factors. Crown lengthening
would give the pt a few more years if age or med history is a factor. Otherwise bone graft and delayed implant.
Sylvia Kowalewski on December 3, 2016
1)Recement post,core and crown,present as a temporary measure with a possibility of infection due to likely contaminated endo .
That will give patient time to make a well informed choice .
2)Crown lengthening would even out the levels of both centrals,endo retreatment (?),new post core and crown
3)immediate or delayed implant
Compare costs of above 2 and 3.
Implants are great but there are also failures and as a time progresses there are all new improvements
Baigalmaa on December 3, 2016
I will suggest option 2 and 7 from your list.
DR A. S. AL AMRO on December 3, 2016
Dear
Thanks for sharing these cases with us
2 option :-
1 extrusion, new casted post and core and crown
2 delayed immediate implant , implant after 6 to 8 weeks from extraction
Swati on December 3, 2016
I will prefer extraction and then graft followed by immediate implant/implant after 3 month.
Amal on December 3, 2016
I would go with the implant replacement after three months
Bruce Deckler DMD on December 2, 2016
Of course carefull extraction graft and place implant is the best solution with a flipper for at least 3-4 months. or extract graft , flipper and later implant. There does appear to be decay in the canal. Nice ferrule maybe extrude and cast post but there appears to be a more difficult preditable out come with implant.
Tilal on December 2, 2016
According to the remaining tooth structure keeping the root is not a good idea because crown length might end up with high gingingival line and poor esthatic so the extraction and immediate bone graft and implant the my treatment choice here.
HY on November 30, 2016
Is the fracture at or coronal to the base of the sulcus? If yes, I would not necessarily do a crown lengthening. I would prep for a cast post – but the prep would have to be tapered in a “V” shape so that the post compresses the root to lessen the risk of a root fracture.
If the fracture is apical to the attached tissue, the biologic width will be violated and then a crown lengthening will be needed.
Patient would be informed that there is some risk of fracture. If the risk is not acceptable to the patient, I would opt for #2 – extract, graft implant. NOT immediate loading. Looks like the patient is a bruxer – there are facets on the incisal edges, so immediate loading would be risky.
JR on November 29, 2016
I have successfully restored teeth in this condition. Some crown lengthening could be accomplished, and actually
improve the gingival symmetry. It looks as though a couple mm’s could be picked-up interproximally for an improved
ferrule, without encroaching on the biologic width. This would have to be done judiciously to maintain as much bone as possible, and with the unfavorable root form in mind. post, and core and of course crown would be redone. The only real downside is losing potential bone for an implant if it were required in the future.
I would let the patient know this would be somewhat “heroic”, and if they had no tolerance for that I would extract the
tooth, place an immediate implant with a graft, and a duraflex temp.. The biotype of this patients gingiva I think would lend itself to implant tx./graft without a untoward reaction, or recession of tissue.
Saud on November 29, 2016
Hi,
I would stay away from fixed conventional bridge as the adjacent teeth are sound and healthy as this would compromise the pupal health so I would go for adhesive single cantilever rather than conventional. If this was my tooth would recommend minimal invasive treatment 1st which is Ortho extrusion of root and new post/core/crown. In worse case senario ,extraction / immediate lmplant placement with no loading/ temp resin retained bridge / restoration and loading after 3 months
Bruce Deckler DMD on December 2, 2016
I like this Idea looks reasonable and promising
Tracy on November 27, 2016
Having dealt with this situation before more than once, I would plan for the extraction/graft/implant. Recement for now, address the lower anterior occlusion via ortho to get those labially tipped crowded incisors in alignment. Then revisit the implant. The majority of the time when these incisors start failing there is an occlusion issue. If it’s not addressed, as you know, we end up with buccal plate and/or fractures. I don’t want the same occlusal forces on my implant.
Noor on November 27, 2016
Hi ,
I would consider the first two options as the best options in my opinion, however, sometimes the patient dislike the idea of implant then I will consider ortho extrusion, new post, core and xrown as the third option as I don’t highly recommend a bridge there, because, the adjacent teeth look like virgin teeth to me (no existing fillings/treatment).
Ara on November 26, 2016
The worst looking tooth is better than the best implant system. That’s my choice. Fight ’til the end.
Doris Ferres on October 23, 2016
If this was my tooth, I would go with option #1. So this would be my recommendation for the patient. My second recommendation would be choice #2. If patient is opposed to implant placement, my 3rd recommendation would be a Zirconium Maryland bridge with feldspathic porcelain on the inner part of the wing for proper bonding. Assuming occlusal stability has been achieved.
Manisha on September 9, 2016
Saving this tooth is not a good long term option. I would extract the tooth and plan for a graft and implant/bridge based on the the patient’s choice. Crown lengthening / orthodontic eruption will not be a good solution because we will alter the crown/root ratio (especially with the decay in the cervical third of the crown). Saving this tooth is not a good long term option for this patient.
S on September 8, 2016
Would you consider another option..short term recement with extrustion if root using ortho which will give you a ferrule as well. Once in suitable position a new post crown and correction of occlusion
Ahlam on September 8, 2016
If aethetics is a major concern of the patient and he has high lip line I would go for immediate implant with bone and soft tissue graft.
If the patient is good motivated with perfect oral hygiene I will do orthodontic crown lengthining for the root ( not surgical ) to keep the gingival outline and gingival zineth then post and core and crown will be my conservative choice
Mouhssine Alj on September 4, 2016
Hi Stephen,
First of all, thank you for sharing your experience and your knowledge.
In my opinion, I remove the remaining dark root, graft and place an immediate implant, for better
esthetic gingival results, and use à zirconium abutment.
Jordan Johnson on August 31, 2016
Recement but have a discussion with the patient that if the crown comes off again a implant will be needed. My pts seem to like having me always try the least expensive route first.
Ron Hickerson on June 26, 2016
1) I would remove decay to see how much healthy tooth I have to work with
2) I would view upper lip line in repose and full smile( it looks like tissue is thick- good biotype for any restoration, not sure about lip line from photo’s)
3) I would evaluate occlusion( looks like anterior wear patterns)
4)) I would discuss options with patient as you have outlined but add
8) thicker post/buildup/crown with minor orthodontic super eruption( or full ortho) and minor CL
If patient really wants to save tooth, is willing to accept risks and has high lip line I would choose option 8 above.
If not, I would extract/immediate implant and stage the restorative temp crown 2 months after extraction with bite guard
Kaung Myat on June 19, 2016
I’d like to choose treatment option 7 if the patient has financial concern. If not, i’ll choose option 1.
Cole on May 28, 2016
How old is the crown?
Was the patient pleased with the esthetics? If so I’d recement everything. It probably just needs a better cement
If patient doesn’t like it…
It’s a little dark under the gum there. I might add some internal bleaching first and then a new fiber post with emax crown
kinjal on May 28, 2016
I would never extract a front and would follow similar line of treatment as you have
Felipe Parra on May 28, 2016
Obviusly I take option 6 cause the x ray shows it ‘s retreat all ready due the Endo -perio and occlusion aceptable condition , an stain tesue Is not always a decay one.well done
Superna Tiwari on May 27, 2016
I would go for crown lengthening.. followed by new post core and crown
Steve S. on May 26, 2016
If the patient is not concerned about the aesthetics of the existing prosthesis and is concerned about cost it would be reasonable to recement the existing post/core and crown.
If the patient wants a better long term option then I would extract, immediate P/- with the view to placing an implant in 3 months.
Either way the occlusion/TMD issues need to be dealt with concurrently.
emilia on May 26, 2016
The last option, new post recemented with the best technique, done imediately or in the lab, cut the gingiva and let it heal with a temporary crown, make a more esthetic permanent crown, in good occlusion and discuss about the possible reduced longevity of this silution. But we have time for an implant later.
dr joe nolan on May 26, 2016
How many of you docs out there actually have a tooth just like this one? I guess zero.
I suffered badly as a kid from appalling dentistry, I own 3upper incisors with this exact scenario, the crowns and posts were done in dental school in the mid 70’s, since then I fractured one from bruxism, had a 3 unit bridge which is still flying along.
So would the implant specialists please tell me what’s wrong with me? BTW, I do place implants too. You guys are in such a hurry with the torque wrench
Dr Luca Paolo Piroddi on May 25, 2016
My opinion is that the option 6 is not a definitive solution because 1) there is no ferrule effect and 2) recementing exactly the same structure that has already failed does not solve the problem.
The option 7 would increase the lenght of the clinical crown of the upper right central incisor having a negative impact on the esthetic unless you would associate it with also an orthodontic traction.
The other options are all doable I would go for an implant (immediate or not) with graft, which is more conservative compared to a bridge in this particular case.
Thank you for the case
Dnyaneshwar Patil on May 24, 2016
My best treatment option is:-
Remove the tooth and place an immediate loading implant provided systemic condition is favourable.
Sumeet on March 18, 2016
I would provide patient with multiple options-
1. Extract, graft, provisional and then implant after 3 months.
2. Extract graft and fixed bridge.
Post and core and recementation does not look like a good option to me.
Najiya Saeed on March 2, 2016
My treatment plan would be
1- providing night guard /habit breaker considering the chipping of anteriors
2-immediate extraction with bone graft and a provisional .
3- occlusal adjustments of upper laterals and
4- implant placement after 3 months .
joe nolan on February 29, 2016
So what’s the problem with offering the least invasive tx, as in clean the crown and recement, either use the existing post or pop a new one
in and line the crown before cementing? It is always best to start with nothing, your patients will appreciate your efforts, even if the tooth is doomed….and how many years was this tooth doing okay for btw?
Just because it is supposed to fail due all the clinical metrics does not mean that it will.
If it fits and fails in a week, that’s ok. All the other excellent options can then be explored.
If there is chronic apical infection or fracture, that’s a different conversation
Arif on January 15, 2016
I would like to ask the patient before decide,what she want to do with your options. But if she is ok with all treatment plans, i prefer to do extraction, give bone graft, place denture, and 5 month after we do implant.
Marwa hakim on January 10, 2016
I will extract the tooth atraumaticaly and place an immediate implant,bone graft, and provisional abutment .
Dr G on January 8, 2016
If the patient was agreeable, I would temporarily recement after removing recurrent decay, provided margins were acceptable. Then do full records and mounting first. Given the wear facets on 21,22,23,12,13 I would need more information on his chewing pattern; to help determine Incisal edge position to permanently restore 11. Repose photo and wear on lower incisor wear pattern and existing anterior guidance pattern study will help to decide this. Grafting with implant would be a more predictable choice given the bone loss visible on periapical radiograph interproximally. The unfavourable crown:root ratio currently would caution me against putting another post/core/crown. The gingival margin is lower on the 21 than the 11, so depending on whether he shows that in smiling this may need to be altered. The question I would be asking is: How long did the existing post/core/crown last and why did it fail? If guidance was the issue then this will need to be sorted in the occlusion design or else even implant option could fail also.
Sanket on December 6, 2015
Considering the long term prognosis, I will prefer extraction followed by socket grafting and then implant
Larry Meyer on October 30, 2015
I have one today at 1:00pm with good buccal bond.
Will extract, immediate implant, and temporary crown.
Larry Meyer on October 30, 2015
Buccal bone
Norberto on October 27, 2015
1st and option with the best long term prognosis. Extraction with immediate implant and loading. Protect the gingival arquitecture with the temporary and deliver a final restoration once the gingiva and the implant is stable and oseointegrated.
Shahriar Sanati on October 27, 2015
Options you gave were basically what I would suggest too apart from a fixed bridge. I find it cruel, out of date and destructive. I only do bridges when it is a redo bridge or neighboring teeth have already crowns, are endodontically treated or need crown for any other reason.
In this particular case I would do a new post. core and crown provided that I can get ferrule without too much lengthening which will cause uneven gum line with the neighboring central.
But but but it all depends on WHO you treating. Predictability is a big factor and with the above option it might not be as predictable as , say, an implant sup[ported crown. So again it depends on the patient’s attitude and wishes.
Thanks again for sharing.
Shahriar.
CPatel on October 27, 2015
If I have my own tooth I would go for post and core crown with more removal of root filling down to apically for a short term option and possible long term plan for implant with grafting .
Also I would prefer to check my excursion movement which creating load laterally and lower teeth
incisal edges of anterior looks worn or eroded so I would consider if any traumatic occlusion.
Robert Tracogna on October 26, 2015
Looking at the PA this tooth appears to have a very tapered conical root with a large endo instrumentation prep. This would put me on guard with respect to the long term prognosis of the root and possible root fracture. This would lead me away from doing another post and core crown prep not to mention that crown lengthening would have to be done to create a long enough ferrule around this tooth. I would not want to create future structural and aesthetic problems by doing crown lengthening in this area.There seems to be some bone loss already between 11 and 21.
If I want to do an implant my next concern is the amount of buccal bone on this root. It’s hard to tell the gingival thickness over the root but the grey shading tells me that it may be thin and therefore may not be conducive to an immediate implant. I don’t want to loose any buccal bone so I may lean towards extraction and bone graft to maintain both vertical and horizontal bone mass for a future implant. Maybe too cautious but it is an unforgiving area of the mouth to restore.
The occlusion is a large part of the equation and this would have to be taken into consideration as far as the design of the final restoration.
Perry on October 25, 2015
I would consider post and core with a provisional for 6 mths to assess ability to handle any functional / bite concerns and strength. Following this I would be more confident in recommending final crown or alternatively extraction and immediate implant insertion to preserve tissues with better long term prognosis .
Angela on October 24, 2015
If it was my tooth: post and crown.
Shahriar on January 10, 2016
exactly!! most of us forget that our object is a human being while giving treatment plan options. I am sure most of the dentist in this tread will do the same as you if it was their own tooth.
Justin on September 25, 2015
i would give the patient 4 options
1. Nothing
2. Extract and denture
3. Extract and bridge
4. Extract and implant
I don’t like to give recommendations to patients as I am biased towards what I feel is optimum dentistry and don’t want them to feel pressured towards it, however, if it were my mouth I would extract and place implant 4-6 weeks post extraction/ simultaneous graft.
Sorin Muntean on September 23, 2015
I would evaluate the broken tooth itself first but I need to see what’s happening also with his anterior guidance.
Why so much flattening of incisal edges of anterior teeth? After that I can take a decision. I’m leaning more toward extraction and implant as a more permanent restoration in today dentistry but in a well functioning system.
Aarti puri on September 23, 2015
Extraction and immediate placement of implant – better long term prognosis
Josh Davies on September 21, 2015
I’m of the opinion that you should try and save natural teeth before looking for replacement restorative options. However it is the cost vs longevity that is the problem. If you think you can get 5 years out of the tooth then go for it! Remember Implants have a lifespan too 🙂
vighnesh on September 21, 2015
Would consider age of patient, ecenimucs of time and money before arriving at a decision
Roberto on September 20, 2015
If it was my tooth I would extract the tooth + inmediate Implant with provisional out of occlusion+ graft; I want to spend money in a long lasting treatment…. With high predictibility.
But if there was a chance to do orthodontic extrusion ( i think it is not the case)… I would prefer that.
Thanks.
Cam Christophers on September 20, 2015
I would prep the canal for a wider post and recement the existing crown and a fibre post . That might last 5 years and would only cost $500 with no biological cost . Depends what the patient wants . I would try to get them to wear a splint
Arif on January 15, 2016
I would like to ask her, which one preferable treatment. If she ok with all of that, than i would suggest to do extraction, bone graft, place denture and 5 months later do implant.
Dr Sheiba Gomes on March 26, 2013
Hi, I am back again , I have just realized that this case was dated May 2011, and the discussion is still on Dr Stephan could you please tell us how you handled the case and what was the final outcome.Thank you for sharing this case and making us ponder.I have also realized that in most cases in day to day practice we are placed in such in situations and each of us finally does what we think is best for our patient ……..
Joseph Kim on March 25, 2013
Using the failed post/crown or fabricating new post/crown does not seem to work without Crown Lengthening or forced eruption to obtain the proper ferrule effect. I guess the lack of ferrule along with occlusal interference on #8 would be the reason of failing of post and crown. However both root expresure procesures does not seem to work again due to conical shape of the root (relative contraindication for CLP) and short length of the root (contraindication for forced eruption).
My choice would be implant rather than conventional bridge or RPD because remaining root and alveolar bone look like perfect candidate for immediate implantation.
Looking forward your explanation, Dr. Stephen.
Thank you for sharing your case with us.
JK
Dr. Ken Miller on March 24, 2013
This type of case is a dilemma in most of our practices. Great comments everyone! Answer depends on so many variables that we don’t know here. Horizontal plane seems lower on patient’s right, is cant of teeth perpendicular to face, I don’t like the shade or shape of present crown or anterior teeth incisal edges, tooth lengths are uneven, does patient want a full make-over or just this one tooth fixed. I’ll assume this one tooth fixed because we don’t have enough information to plan a make-over.
To fix the right central incisor I would remove the decay and excess gutta percha above the 5mm necessary apical gp. I would bond in a proper fitting quartz fibre post and build up a core and do an Emax crown. I would do a slight gingivectomy to raise the gingiva above the right lateral and central incisor to make their tooth lengths in millimetres the same as the left lateral and central. I am just making the four anterior teeth display the same amount of tooth not fixing the slanted horizontal plane. From the look of the radiograph, there is enough biologic width above the bone that I could prep the labial margin of the crown a little more cervical and cover up the dark root with a new crown. Of course I would need to sound to bone after the gingivectomy to determine that. I would probably aesthetically re-contour the anterior incisal edges to make them look better. This would be my minimum treatment for this case and the patient would be well informed of its compromises and unknown longevity.
If they wanted a more permanent solution and money was not an issue, then I would extract and do an immediate implant with slightly lingual placement to allow a screw-retained abutment/crown with an immediate temporary to preserve the papillae. Bone grafting would be necessary to fill in between the labial plate and the implant. Again, at time of permanent crown abutment placement I would consider slight gingivectomies and incisal edge recontouring to make the result more aesthetic.
My answers only handle this one tooth and slightly improve aesthetics. IF the patient wanted a full make over, we need more information.
I would do a quartz fibre post because the root would fracture sooner using a metal post (no flex to them). I have not heard much about bleaching or whitening roots in a case like this. My endodontist tells me I need to seal the top of the gutta percha before whitening or the apical seal will be ruined by the hydrogen peroxide. In this case I think it would be hard to place a sealer filling or cement plug in the canal, bleach the root and then remove this plug to bond the post in place. Hence my reason for prepping the crown more cervical to try and hide the dark root. I wonder if one could use the “Dickerson Ditch” technique here. Dr. Bill Dickerson of The Las Vegas Institute once promoted drilling a small prep in labial portion of the root 0.5 – 1.0 mm in from the labial surface and filling it with white composite to improve the look of a discoloured root. In this case it may weaken an already over prepped root.
James B. Graham on March 23, 2013
Nice case presentation. I would like to see photos of 1) natural smile line, 2) high smile line to see the relationship of the upper lip position relative to the teeth and gingiva, and 3) MI position of mandibular teeth to maxillary teeth. But, from the photos presented, I can see a discrepancy of the lengths of #7 and #8 being clinically shorter when compared to #9 and #10. On the patient’s right side, the teeth appear more square (esp #8). There should be a 1.2/1.0 length vs width ratio for proper esthetics. In this case, it appears to be a mix of gingival architecture and incisal wear. I would need measurements (clinically or from Dx casts) to establish the proper crown length ratios and the extent needed to create a natural appearance. This could possibly require crown lengthening to the first bicuspids depending on the patient’s smile line. The advantage of this case is 1) the #8 endo appears adequate (depending on exposure time to saliva that the crown was loose), and 2) you stated the case was periodontally healthy. The down side is the length of time necessary (4-6 months) for tissue maturation prior to placing retraction cord for an impression without causing gingival recession.
I would “rack & stack” the proposed tx options as follows:
1) esthetic crown lengthen anterior sextant, cast post & core, crown* (my highest recommendation for this case)
2) remove #8 with immediate or delayed implant/crown
3) remove #8 with RPD with ovate reinforced acrylic pontic**
4) remove #8 with FPD w/ovate pontic (with or without esthetic crown lengthening) (my lowest recommendation for this case)
* occlusion info needed to determine ceramic or metal ceramic crown (if a ceramic crown can be used, then I would use a metal ceramic alloy for the cast post & core, then place opaque porcelain on the core; a zirconia post & core is white and I would prefer to have control of the core shade)
** an anterior RPD single tooth can be often difficult to match; if needed, select a porcelain denture tooth, cut it back facially, the custom stack it with aluminous porcelain used for ceramic crowns, then process into RPD
Cliff Leachman on March 23, 2013
Crown lengthening, gold post, new crown and night guard and warning.
Implant may reorganize the tissue negatively making the crown lengthening
the superior choice. ortho extrusion if you don’t have enough ferrule.
In the right hands the implant is the appropriate treatment, but not all
Clinicians can place anterior implants and create ideal gingiva.
That’s excluding the single most difficult restorative situation a single central crown.
Kunle on March 23, 2013
In addition to the 7 listed options I would consider refining and inserting a new post and core build-up followed by non-invasive adhesive resin-retained crown build up with a provision that the patient should keep-in-view a graft/implant/crown option in case of a failure in the future.
alan slootsky on March 23, 2013
WHAT ABOUT THE FX AT THE BASE OF THE POST GOING TOWARDS THE DISTAL?
AND ALL THAT DECAY DOWN THE ROOT?
CONFIRM ON CONE BEAM–
GIVE THE PATIENT THE BEST OPTION ONLY….
WHICH IN THE LONG RUN, HAS THE MOST VALUE TOO.
IMMEDIATE LOADED IMPLANT–ONE PIECE SCREWED IN… WITH PEEK ABUTMENT
THE SUREON CAN MODIFY THE EXISTING CROWN FOR THE TEMP
IT WILL PRESERVE THE SACRED PAPILLA
IF $ IS A PROBLEM, WAIT TO DO THE FINAL RESTORATION
Mojdeh on March 23, 2013
The best option for him if there isnot financial problem,
Ext. The root and bone graft+ implant at the same time.
Fahd on March 23, 2013
Since the root filling seems alright with good apical seal. I would go for the crown lengthening and remove the gp on the wall in the coronal 1/3 because screwing in the post to the gp wall wouldn’t give good retention for it. And then go a bit deeper with gates glidden leave 4-5mm of gp. And go for a custom made post instead of the preformed one they’ve used ealier. very reason it failing.while this is going on maybe the patient can have a provisional RPD.
Joselito Y Carreon on March 23, 2013
the root canal looks over prepared going up to apical 3rd and can cause a weak root. Place RPD while still undecided on the type of fix restoration.
Dr Sheiba Gomes on March 23, 2013
I read the various treatment options: Ineed to know about the occlusion, the age of the patient,whether the patient has a high smile line? Success would depend on taking care of the occlusion primarily thereafter moving with the other considerations and yes I would definitely recommend a CBVT prior to any consideration for an implant.
Teresadds on March 23, 2013
There is more than enough distance between the crestal bone level and the margin due to horizontal attachment loss so crown lengthening is not necessary but gingivoplasty is indicated and there’s enough space Gallery 78 street: 43 E 78th, 6-9pmto establish ferrule without violating the biological width. There’s about 5 mm space from margin to bone crest so I would remove all decay and prepare for cast post and I may or may not use the existing crown depending on esthetic requirements and occlusal clearance. Implant is also an alternative but aesthetic result could get tricky for anterior teeth.
Peter G on November 26, 2012
A lot of good points have been made above. Personally if there is any gingival display at all and given the discoloration of the marginal gingiva (shine through from the dark root) AND the fact that the soft tissue margins are uneven with the tooth in question being shorter, I would recommend extraction and carefully placed immediate implant. This could be done with or without immediate temporization which I believe is showing promise as preserving the most vertical hight of both bone and soft tissue if done properly. In this way the free gingival margins could be leveled, the shine through alleviated and bone preserved for the long run. A new post, core and crown is conservative in the short run but not if the root fractures down the road. Almost certainly this type of restoration will fail given enough time with the history eveiden for this tooth. Crown lengthening would almost certainly result in a black triangle issue…
Skip Jeranko on November 19, 2012
It appears that the root itself is still intact and is not cracked, and has the potential to be restored if the patient wanted too. My question is, does the discoloration of the root bother the patient esthetically? And what is the occlusion like on the tooth? If the patient has good centric stops and anterior guidance is distributed over several anterior teeth, then there is a good chance of success by placing a new post that goes farther down the root, ideally 2/3 of the length of the root, and is a little wider so that you are not on gutta percha but sound root structure instead. Then re-prepping the tooth for a porcelain crown that goes more subgingivally and is more esthetic. If the root discoloration bothers the patient, then the implant or bridge would be the best choice. Still the occlusion needs to be checked either way.
Julio on November 18, 2012
Bring the root coronally with braces to get the ferrule effect and make a new post and crown
Peter Pagano on November 18, 2012
Stephen, Great case for discussion of treatment. I recommend a cone beam 3D image of this area be taken to check two basic things: 1) the triangle of bone volume surrounding this tooth per Dr. Scott Ganz.This data is invaluable in determining the labio-lingual tooth position and how much labial and lingual bone is present if planning an atraumatic extraction procedure, GBR, GTR and immediate or delayed implant placement. If a truly restorative driven approach is planned a radio-opaque idealized tooth can be included in the 3D scan to impart data about the implant fixture’s trajectory as well as the abutment’s emergence trajectory for the idealized provisional crown and final implant crown. This approach allows for a decision tree based on more data than a 2D radiograph can provide.
2) There appears to be a lingual crack in the root of #8 (#11). A cone beam radiograph should be be employed to determine if it is a crack and the extent of the crack prior to presenting options or proceeding with a course of treatment. Just a last thought: I heard this from Dr. Scott Ganz. “Cone Beam CT is presently state-of the art technology; however, if one is sued it becomes the standard of care.”
mathew on November 18, 2012
would prefer ortho extrusion, implant placement delayed, occlusal equilibration.
Chris on November 17, 2012
Just curious as to whether all 7 options were presented with corresponding costs of tx the same time or did you present options and give costs later?
James on November 17, 2012
I purposely did not look at any other comments above. All of your options could be valide but I am missing important information to make a specific judgement as to my preferred treatment.
Age , What is cosmetic risk? No smile photo of face, why was the tooth crowned in the first place. is tissue color relating to poor margin or a biologic width invasion ? Radiograph leads me to believe poor margin and not biologic width problem , I would freeze and sound to bone before final decision. With the limited information I have I will make some assumptions maybe correct or not . Assuming high risk cosmetics ,younger age, tooth was damaged due to trauma, low generalized biomechanical risk other than this tooth. I can not see any other restorations present. in the photos. If patient is younger there is cuspid wear, age appropriate or not?
This appears to be inside to outside wear pattern suggesting bilateral bruxing ( sleep disturbance) or central mediated parafunction placing patient in high function risk category. wear on #10 as well as ,#7,# 9seems to match notch on lower. Never the less parafunction has to be considered. I am not sure in your system what you call that.I would choose an implant . If younger and trauma induced this tooth even with a RCT this tooth can do some strange things over the next years. With post and core that has alrady failed and wide canal i think this is a singnificantly weak tooth. If biologic width invasion bone is high crest improves this implant. If you crown lengthen to achieve appropriate soft tissue placement and gain ferrule effect you are taking away vertical bone height that you might need for implant if fails again or external internal resorption happens at later date for this patient. The interproximal bone on adjacent teeth will hold interdental papilla and you can improve distal papilla because of the roots of #7 and #8 with properly placed implant. Crown contacts less than 4-5 mm coronal to bone will fill in predictably. Need 2 mm facial bone for immediate placement. Be sure to place long axis of implant slightly lingual to incisal edge better to err to lingual than facial. good cat scan can give you this info . Place crest of Biohorizons lazer lok at 2mm below where you want free gingival margin to be.
This is a great case for why patients get confused when going to multiple dentists there are many ways to look at this example. Does not mean anyone is wrong . We all have our biases based on individual training and clinical expeierence. I am trying to drive this tooth away from the biomecahnoical risk and improve the soft tissue appearence at the same time. Hopefully improving the long term prognosis for this patient. My worthless 2 cents.
Ed P on November 17, 2012
PS forgot to add. Even with the implant, you must fix the lower anteriors first.
Mircea on November 17, 2012
Hello everyone
Great to have a chance to communicate with so many people on this wonderful website. Regarding the case, I would like to start with one thought:”WE , AS DENTISTS, WE ARE JUDGED ONLY BY THE LAST ACTIONS WE HAVE MADE”. It does not matter what wonderful things you had made for the patients in the past, if the last one does not meet (or exceed) patient expectations, your credibility and reputation hardly built in the past will be compromised ( in seconds!). This is the reason why I do not think that saving this root will be a viable option.
– recementing the post will not solve anything, does not matter the cement you use , risk of decementation an/or root fracture will be higher, with potential complications on buccal plate.
– crown lenghtening will have serious esthetic complications, even if ferrule effect will be improved. We have to go on left central as well , making the things more messy
– ortho extrusion will compromise crown /root ratio , we have to do a crown lenghtening anyway , if ortho extrusion is done slowly and the root will come down with the bone and gingival tissue
– no matter ceramic and post we use , there is a risk for dark root surface showing through, depend of attached gingiva thickness.
Remember, after so much money and time spent , patients they forgot from where they left. The “arrival” point maybe will not be the one expected from esthetic standpoint. Even patient had this darkness show through in the past without bothering , probably will point at this issue at the end. And maybe you may suggest a gingival graft, another procedure….
The only reason for ortho extrusion ,I think, is only to bring bone down for implant placement and papila support. It looks that the bone level adjacent teeth is fairly decent and papila may have fair support after grafting. Immediate implant placement with good contour temporization could be an option as long as we can achieve primary stabilization. It is more unpredictable though, I prefffer 2 stage implant with grafting.But this depends only from doctor personal prefference. Zirconia abutment and all ceramic crown can take care in most part of root darkness. Temporization in different ways with flipper , Essix or an adhesive bridge can take care of papila support. Critical is atraumatic extraction and grafting.
Occlusion -wise , is not ideal, but it looks that patient can be equilibrated. If lower incisors can be recontoured to have at least 2 points of occlusion in protrusive movements will help. Canines they show some sign of incisal wear. If there is no complete disoclussion posterior in lateral movements , we can add some bonded composite inciso-palatal ,without invasive procedures. Critical is implant adjustment in centric and eccentric . Finally a nightguard will help, preferably an E-appliance.
It is very important that the patient will know from the beginning the limitations of the procedure, including esthetic outcome. Setting proper expectations is very valuable. But in the final, remember, for people the most important is a longest lasting treatment. They don’t want to come back for the same problem and usually they forget that we tried to do the best or conservative at a given point. Even if you document and discuss with the patient everything, in their mind is only one result ” my dentist did a treatment which failed too soon”.
David Gibson Dds on November 17, 2012
Obviously an implant is the best long term option, Even though the other presented options are acceptable. My advise Give, the patient a chance to say no to the best..
Ed P on November 17, 2012
There are great comments here. I could not take the time to read them all but I like Mark’s and Joes up top. It is all about risk vs reward and the patient’s values and limitations. IF we are discussing this purely from a clinical perspective and we wish the result to be esthetically idealized, then the lower gingival height of 8 needs addressing with CL. That, however, will compromise root length and stability as the apex, relative to 9, is shorter and tapered. I also worry about the integrity of the root in so far as the diameter of the GP fill is extraordinarily broad and that took at least twenty percent more structure away from the body of the root. The lowers are a primary reason why the crown loosened. Do the case without addressing that and it will fail quickly (been there, done that). The root did not fracture because the post was buffered by all the GP. Bonding it well to the root surface would increase the stresses on the root increasing fracture potential an indeterminable amount. All said, if one considers a 5 year success rate as satisfactory, with the option of an implant after failure, then that is a good, reasonably cost effective, short term solution.
IF your wish is to do it once and be done, and if then a good implant works.
But this is real life so YOU MUST FIRST ASK THE PATIENT WHAT THEIR VALUES AND LIMITS ARE. Then act accordingly.
Robert on November 17, 2012
There is yet another option: orthodontically extrude the tooth, then restore. You must findo out what the patient wants as all are good treatment choices. You should ask yourself the question, in my mouth what would I want done?
Galina Mayer on July 20, 2012
Stephen is very cleaver, it looks like he concealed a lot of information, but if you really think about it, the most important info is provided.
As always with case acceptance (my favourite topic), BEFORE we come to tx. case presentation hopefully we gathered HOW pt is thinking, WHAT’S IMPORTANT TO THEM, how much time they are prepared to invest in the treatment, and what is their financial situation. After knowing all those, there may be no need in discussing ALL 7 tx. options and their advantages and disadvantages. After all, we are not looking into converting a pt. into a dentist! and we don’t want to confuse pt. too much.
Although pt. seems to be fairly young they have tremendous wear on ALL upper front teeth, including both canines which are worn to the point of dentin exposure, and I suspect that it is on the lowers as well, especially on right central and lateral under the porcelain crown. There are crack lines on central and laterals, some G. distress as a result of occlusal trauma, and G. assymetry (left lateral is higher than central; canines and centrals are not alighned) and of course, assymetry between two central incisors. So this is not a one tooth dentistry, but a full mouth dentistry case.
G. assymetry and dark ‘show through’ may not be an issue aesthetically as the upper lip may be covering it (low frenum attachment?), and shape assymetry between two centrals can be fixed easily during the restoration process.
To be fair to the previous dr. it is not easy to produce a perfect crown on single central, but if all front teeth will be restored it will be easier to control the colour and shape, and if the full coverage will be chosen, the fixed bridge situation will make sence, wether you extract the root or leave it burried.
If the pt. has a high smile revealing the gingiva, both of the centrals could be crown lengthened to create a better proportion
After listening to Dennis Tarnow at our last Crown and Bridge meeting I suspected that you will be placing an implant there, Stephen!:).
If the implant is chosen [which means that pt. does not have an aversion to Titanium & the pt. is not a dentist ? 🙂 who feels strongly about keeping the root of the tooth], and if the periodontal condition is compromised, the ortho extrusion can bring the bone down first, and then root can be atraumatically extracted, bone level adjusted, and implant is placed with or without grafting. Some type of ceramic abutment may be chosen to mask the dark ‘show through’ if it is visible.
I guess with this case Stephen wanted to show us to look beyond this one tooth and at the whole mouth and the whole face, and how to rise above what we believe for ourselves and how to find and offer comprehensive solutions.
Great case, Stephen! Thanks
Galina
Dr. Jeanette Garner on July 19, 2012
Hello from my holiday sailing in Mallorca! A’s the gumline looks fine and healty, and the post luckily went out, I would not hessitate to prep for a new laboratory made post buildup i strong metal ,after that a porcelain Crown probably an emax. If anything goes wrong I would concider the more drastic procedures , but the gumline in the front are always my biggest concern, and you know what you have , not what you get!
Best regards dr, Jeanette Garner
Arshad on July 19, 2012
You have a good band of attached gingiva. Also the level of gingival margin on #8 and #7 is lower than #9 and 10 so there is a good potential for crown lengthening. However what remains to be seen is how much tooth is left after caries removal. Ideally, we need 1.5 to 2mm ferrule.
DR TWIN on July 19, 2012
DID A COST COMPARISON AND PROGNOSIS NEUTRALIZE TREATING THE TOOTH VS AN IMPLANT.SAME COST AND PROGNOSIS BETTER IN LONG TERM FOR IMPLANT
Dr Stephen Phelan on July 18, 2012
Hi Everyone,
Thank you for all the great comments! I will share with all of you that after consultation the patient decided to remove the root and have a dental implant placed. Stay tuned and I will share with you how I managed this treatment plan to achieve an excellent result for the patient.
Best regards,
Dr. Stephen Phelan
Dr.Mercede on July 18, 2012
As i always try my best to keep original root and as it seems in the x-ray that the root and periodontal tissue is healthy, my first treatment plan is to remove residual decayed structure then prepare a new post and core and place a new crown on it.
Dr. Shikha Goel on July 18, 2012
It will be best to retain the patient’s original root. I would like to excavate residual decay, followed by crown lengthening, remove any extra gutta percha within the post space leaving a 5mm apical gp with a leveled surface. i would then take a post space impression for cast post and core followed by full coverage crown.
DR TWIN on July 17, 2012
CROWN ROOT RATIO VERY IMPORTANT IN ADDITION TO THE VIOLATION OF BIOLOGICAL WIDTH AND THE LACK OF TOOTH STRUCTURE TO ATTACH TO. WITH OUT A RADIOGRAPGH I WOULD PROBE FOR SINUS TRACTS AND WITH A RADIOGRAPGH DETERMINE BONE HEIGHT AND VITALLAITY OF BUCCAL PLATE ,ROOT FRACTURE AND APICAL VIALABILITY, THE EXISTING CROWN CAN BE RECEMENTED WITH TEMPORARY CEMENT AND ATTACHED TO ADJACENT TEETH WITH GLASS SPAN AND RESIN TO REINFORCE THE TOOTH UNTIL A A LONG TERM FIX BOTH POSSIBLE AND FINANCIALLY CAPABLE CAN BE DETERMINED BASED ON THE NEEDED MEDICATIONS RESULTS AND HEALING PROGNOSIS CAN BE EXPLAINED. THE TOOTH IS NOT RESTARABLE AT THE CURRENT LEVEL OF ROOT STRUCTURE SO CROWN LENTHENING WOULD HAVE TO BE CONSIDERED IF POSSIBLE CONSIDERING ESTHECTICS OF GINGIVAL HEIGHTS,SECONDLY I WOULD NOT PRESENT ALL OPTIONS UNTIL PRESENT EMERGENCY IS RESOLVED, A FLIPPER MAY BE CONSIDERED, OR PUTTY TAKEN TO PLACE OVER ROOT WITH CROWN IN PLACE TO MAKE TEMPORARY BRIDGE IMMEDIATELY, THERE ARE MANY POSSIBILIIES, RECORDS SHOULD BE TAKEN TO KEEP ALL POSSIBILITY OPEN, EVEN BONE AUGMENTATION AND IMPLANTS, CALIFORNIA BRIDGE, CROWN LENGTHENING, CAST POST CORE AND CROWN,SHADE TO BE DETERMINED IF NEEDED 3 WEEKS AFTER BLEACHING,PARTIAL DENTURE, FLIPPER, DENTURE, YOU HAVE TO LOOK AT THE ENTIRE MOUTH TO MAKE A DECISION , AND ALWAYS CONSIDER THE BITE,MEDICAL HISTORY, DESIRES OF THE PATIENT AND YOUR OWN LIMITATION AND OF COURSE THE THE TEAM OF SPECIALIST THAT YOU UTILIZE FOR CENTRAL COORDINATING DIRECTION AS THE PATIENT PRIMARY PHYSCIAN WHICH SHOULD ALSO BE COORDINATED WITH MEDICAL PROFESSION,WIH THE RELATIVE SPECIALTIES COMMUNICATING WITH YOU AND THE FAMILY PRACTITIONER.
dr shabnam on July 17, 2012
Hello doc ,
According to your brief description about the case it seems the root is intact and not mobile … recuurent caried present ?but if hard then i think it can be considered arrested … We can repeat the post and core and do it properly again ,with a good post lentgh within the root and good built up core . a crown can be placed .
owever if bone loss around the cervical portion is more then beeter extract the root piece and go for an implant … if patient can afford ,..else the classical bridge zirconia crowns etc ..
Dr.VJ on July 17, 2012
Start with a better preparation of the post hole since I don’t see any problem with your RCT and you have a good apical seal.I would prefer a casted or custom made post and core with improved ferrule for greater retention of the crown.Crown lengthening is an option to improve the marginal esthetic of your crown comparing it with the marginal gingiva of the contralateral central incisor.
Natalia on July 17, 2012
I would prefer to try a less radical method as tooth extraction can be done anytime. One of the most important part in the future restoration, not to mention the tooth strenght, is the recovery of the aesthetics in the gum area. So, I would remove all the dark colored dentine and restore the tooth with a fiberglass post fixed with a compomer applied in as many layers as possible. After that I would make a direct composite restoration.
Dirk.C.Deutekom on July 17, 2012
From the Netherlands:A lot of opinions: I probably go for first saving the root and apost an core( fiber/composite) and a new crown .
If the ferule is not wide enough some crownlenghtening procedure and perhaps try bleaching the root as it is shining through .Consider also what an implant would do .
If you do a lot of implants in the practice you would consider that earlier in your decisionpath .
That said I have seen a lot of esthetically soso implants in the front
A “healthy “root is still the best implant in my opinion
Lena on July 17, 2012
I’d go for extraction + implant (immediate or delayed), as there’s decay already starting in the root. Why use the root again only to get the patient come back to you after some time with the same problem when the decay has developed further? The periodontal structure might be good (for the time being) but what would be holding the post in place is the root itself (with the help of cement/gutta percha, of course) and as decay develops, the structure would become loose and the whole case would repeat itself.
That is, of course, what I’d opt for. But if the patient chooses another option, well, it’s their teeth, so I’d do as requested.
Syd on May 25, 2011
Nice post and a common situation as well. What did the patient end up choosing?
Seeing the smile line will be important here and knowing the patients esthetic and functional expectations will also be important.
i agree with the comments as to wanting to know why it failed? flared lowers constricted envelope of function etc? this may need to be addressed with ortho as well (someone mentioned invisalign)
There’s not enough ferrule for a post and core unless something is done: ortho extrusion/ crownlengthening
And how will that look if it is a high smile line? and is it still out of functional occlusal risk?
Then what what becomes the prognosis longterm…
For extraction:
1) There is always the bridge option, Bone (preferrably slow resorbing) and tissue grafting then bridge.
2) Implants : delayed or immediate.
When I looked at the xray ; it was unclear if there was enough adjacent bone level interproximally on the distal….if there wasn’t … there would be a high risk of “black trangle” and loss of a papillae looking tissue distal to the implant site. This would happen regardless if delayed or immediate.
If there is enough bone on the mesial of the lateral (1.2) … One way of a delayed option would be to extract wait about 6-8wks then place the implant; graft if necessary.
If there isn’t …well… you could try ortho extrusion–extraction to try and grow bone as best you can.
Many options but I believe the risk of the procedure , the risk the patient is willing to assume,, and the expected longterm prognosis will play a role
Stephen Phelan on May 19, 2011
Hi Everyone,
Thank you for all of the great ideas and comments. I am at the AACD meeting in Boston and just spent the day listening to Drs Dennis Tarnow and Stephen Chu which relates well to this blog post.
I will create a follow up post next week with the treatment option that the patient decided on and how I executed the treatment for her.
Thanks,
Stephen Phelan
Kennedy Mascarenhas on May 19, 2011
The patient has to be definitely explained all the pros and cons for all given options
I would prefer a cast post and a crown as a 1st option and implant therapy as second , while considering the occlusion including the wear facets for which is a night guard is must …
In addition following factors have to be considered :
1.Remaing tooth structure should be hard
2. Canal Diameter: The canal diameter in the coronal 1/3 appears to be half that of the surrounding remaining tooth structure. According to the proportionist theory, canal diameter should be 1/3rd the remaining dentin
Therefore considerations should be given for reinforcing the first few millimeters with composite resin along with the anti-rotation feature before making a direct pattern or an impression for the fabrication of cast post
3. Ferrule: Ortho extrusion with Crown Lengthening Procedure (CLP) would be great, only it would be more time consuming and temporization during extrusion could be difficult.
As we do not know the smile line, in this situation palatal ferrule would be more important than the labial ferrule. The amount of tooth structure from the marginal gingiva palatally, cannot be appreciated in the photographs. Therefore CLP may be considered only on the palatal aspect, even if the patient has a high smile line
Doug Jones on May 19, 2011
Great idea for a post- so many choices
There appear to be signs of bruxism/ parafunction – heavy wear on adjacent anterior teeth. What do the lower anterior teeth look like. Is 41 contacting prematurely either in centric or in protrusive excursions?
If there is a high lip line aesthetic risks are high. If not, then I would lean towards crown lengthening and a new post and crown after addressing any occlusal contributing factors.
Re-cementing the post and crown is likely a short term solution – definitely high risk of failure especially if the occlusion is a contributing factor. And in doing this, the option of a redo could disappear with a root fracture or recurrent decay after the re-cement.
Making a new post and temporary crown with ortho extrusion to enable a ferrul makes sense to me. Still, the patient must appreciate that this is also high risk.
If there is a low lip line then the extraction, bone graft and immediate implant placement is also a viable option.
Definitely a night guard to protect 11 and the other anteriors from further wear.
If the risks and benefits are explained and the patients questions answered, I believe the patient will contribute information about their values, expectations, lifestyle, needs that will enable the dentist and patient to arrive at an acceptable decision for the patient . This is a dynamic conversation that will require both the patient and dentist to listen carefully to each other to discover the win/win solution.
This is an excellent example of how a formal informed consent form with complete documentation of the conversation is so important.
DJ
Dr. Gary S. Ford on May 19, 2011
Great post as usual Stephen and you have received multiple responses, which is not surprising. A picture of his/her smile would have helped an awful lot and guided our decision making. Did he/her express any dissatisfaction of the previous crown and the “show through” (which I would not mention if it was not brought up) or was it acceptable?
If it was acceptable – cut to the quick and just redo P&C/PJC. Crown lengthening, I feel is not required as you can go a little subgingival without compromising the tooth – but if you really felt the need to do “gum gardening” it would have to be 12-22.
If the show through was a bother to the patient – extract, graft for ridge preservation. Immediate surgical placement of an implant depends on how well you can pull out the root without destroying the bone architecture. I prefer delayed placement. On an immediate placement, how long do you wait before proceeding to the final crown?
Root fracture – doubtful but it is a Dentatus screw and highly suspect, but as the radiograph suggests it was cemented to GP. Redoing the post with leaving only 3-5mm of GP, you would get better retention for the future crown. I would probably go with a cast P&C as the discolored root itself is causing the shadow. Crown – PJC – a pressed ceramic but not a PFM, I haven’t been too impressed with zirconia but hey, lets wait and see the incisal wear with that type of porcelain. My bet is on the porcelain.
Ortho extrusion – nope, no way, not required, not unless I had an “unexpected” tax bill that I had to cover (just kidding, we would never do anything like that!)
Maxillary bruxism appliance – most likely and depends on other pathological S&S and the patient is displaying incisal wear and flattening of all cusps.
Reimbursement if fails in less than 5 years – never. Takes all the onus off of the patient and puts it on me – no thank you. As Gordon Christianson once stated “we have to stop selling dentistry that lasts a life time – nothing lasts a life time.” and where is the patient responsibility in that equation? The overall prognosis of this tooth from the start was poor, so any remaining time you get is a bonus whether it is a year or two or five. By the way that reminds – how old was the P&C/PFM? age of patient? did you recommend he/she go and get a “refund” from the previous dentist since it “failed” (again just kidding – code of ethics, RCDS(O), etc. – messy messy business, better leave that one alone).
Bridging the gap – hard to recommend that one, cutting down on two almost “virgin” teeth – shudder, cringe. Besides, just what is a “virgin” tooth? Did you hear the one about a lawyer suing because the dentist never recommended an impant…..
So, Stephen, how did the implant go? I know the kids, especially your son the pirate, wanted to go to Atlantis and you just had to stay in that mega luxurious apartment, didn’t you? Again just kidding – but life does have a way of directing our dentistry….
All the best and I look forward to the replies.
Roger Harrington on May 19, 2011
My lean would be to recem existing post and core on a temp basis, then crown lengthen lateral to lateral to get a nice architecture. Following adequate healing time, fabricate a cast post and core with anti-rotational feature and new crown with adequate ferrule.
I like Paul’s plan for extrusion but wonder about asymmetric emergence patterns in two centrals??
PJ on May 19, 2011
Depending on the patients finances and how good your lab is and comfortable they are doing it, I have had a similar situation. You remove the excess GP, prep a ferrule and hve a new cast post and telescoping coping made to fix the existing crown. You may need to adjust the margins to accommodate for aesthetics, but here they are subgingival so a thin gold band on the facial shouldn’t show.
Dr. James Miles on May 19, 2011
Great post Stephen. I see healthy tissues and a compromised tooth with an apparent history of early successful endodontic management. I suggest that the remaining root structure will not offer long term stability and to due crown lengthening to achieve a ferrule for retention may provide an immediate technical solution but long term periodontal management issues in an esthetic zone.
I feel the best option would be to extract the root and graft the area while using a RPD to develope the gingival architecture. Revisit the healthy area with a two staged implant crown restoration with the normal consent clarification around these procedures.
If the patient is not in a position to chose this option, I would suggest a compromise treatment of placing a cast post/core ( I would do a modest internal prep of the root for anti rotational purpose) and cementing this with C&B Meta Bond. I would have the buccal aspect of the post/core cut away so that I would achieve a porcelain margin to minimize any “glow-through”. I would stress to the patient that this would be a secondary option and I would not place a “time” expectation on this choice. I also would not institute a future “credit-towards-alternative treatment” beyond one year. This is a secondary choice and requires the patient to assume a greater level of responsibility. Having said all of that, I feel both procedures would require a Night Guard “back-up” not withstanding our ability to work within this envelope of function. It just appears that there is an Incisal wear issue but I need more info to visit that subject.
Thanks to all of you for your insights
Paul on May 19, 2011
I have done this many times with good success. place a new post and core in the tooth and bond on a temporary crown. then use ortho brackets to passively erupt the tooth until you get our 2-3mm ferrule. then you can reprep for new crown. this should only take a few months.
Yves Ayotte on May 19, 2011
We know litle of the patient, sex, age… The abrasion seems to indicate a fairly agressive occlusal function. The XRay indicates a normal periodontal support and a good reaction to the endo ttmt. The post is not proper as it is mainly in gutta percha. There may be a fracture line at the apical third that would need to be evaluated with another Xray (different angle).
If I agree that the ideal treatment in the case of a normal occlusion pattern should be an implant with all the du consideration to esthetics (which could be a problem ounce the root is extracted) and double price tag. I would certainly consider redoing the crown and post with a properly prepared post and adding a long bevel to the crown to give a bit of ferule effect if the patient seems limited with $$$. I beleive that if the occlusion can be controlled and the root is not fractured, the crown and post could be a viable solution.
Joe :) on May 19, 2011
Thanks for sharing this Stephen.
Regarding immediate choices, recementing the original is obviously convenient. Even with permanent cement II don’t think it will hold for long and the patient could be lulled into thinking the situation was solved.
Like Lyn said, that old post was just engaging in gutta-percha and it still held for a while. That bodes well for getting mileage out of a new post-core-crown option.
Lyn’s suggestion of offering a refund if it breaks within 5 years sounds like crazy-talk to me. This tooth is vulnerable and the longevity would be questionable. The patient would have to “baby it along” to ensure decent longevity.
I’m curious about the upper lip line (no smile shot here). Preserving the gingival architecture becomes a priority with a high lip line.
The patient has an unbalanced incisal line. Could this be a multi-tooth or Invisalign case? Those lower incisors look flared and would put extra stress on #11.
Any budget concerns aside, I’m leaning towards option #7. Looks to me like it’s worth a shot saving that root. The crown lengthening could even be done on both centrals to give that little extra extension and recover more ferrule on #11.
Putting the original post-crown back in with temporary cement would be appropriate if the treatment direction was a new post-core and crown. I would want to act fast on the new post-core so the old one wouldn’t become a problem by falling out. A final crown could wait until any crown lengthening was completed.
Joe
Kelly on May 19, 2011
You could make a new post/core/crown but advise the patient it may not work. Crown lengthening would be hard to do because you would end up with esthetic issue with the tissue. I would not do bridge or RPD. I think some type of implant placement is best, either immediate or 2 stage. (need to look at where the lip line is). Another option I have seen is orthodontic extrusion then restoration but I think maybe that is a little heroic. Implant placement I think is still the best right now because there is no root pathology and as long as there is enough bone to work with I think that would be the best long term.
Mark safari on May 19, 2011
I would go with same options but instead of bridge I rather to make a new post core crown without crown lengthening and leave it there till it breaks.With new bonding agents and cements and posts it will be better than it is now.after all it has been there for years and it may work a few years more .It’s perio looks good so I will not do the crown lengthening(if patient decided to go with crown) and if I make it off In protrusive movements specially if it is female I think is a better option than bridge.
thanks
Lyn Fitzpatrick on May 19, 2011
It appeaars to me that thte post is sitting in the midst of a lot of gutta percha. I would give all of the options and reccomend that we try to reuse what is there with some modifications (get rid of the gp and recement). I would tell my patient that this might not work and that we may have to move on toanother option if it fails. i would remove the tooth from occlusion. i would also inform the patient that if this treatment fails within 5 years I would apply the costs spent now to the subsequent treatment. i think that is fair and the least invasive option
tomer on May 19, 2011
well, first of all i would liketo see an X ray to find out if there is any reaction in the apex of the root. If everything is fine, i would prepare the root for a DCR ( which basically means in romanian: dispositive corono radicular). In this treatment option the patient get to keep his “original” root and give him a better feeling in the treatment. I personally think the majority of the patients would prefer this kind of treatment, of course if it is possible to do so.