- Home
- keyboard_arrow_right Phelan Dental Seminars
- keyboard_arrow_right Part 2: Would you extract this tooth or not?

Hi everyone, I wanted to start off by thanking all of you for the excellent ideas and comments related to last weeks post. Many of you had excellent ideas about how you would treat this patient and today I would like to share with you the actual treatment plan the patient selected.
As I explained last week, I listed the options that I thought were reasonable for this case and the patient let me know that she wanted a predictable long term solution and that she did not like the grey that was showing through her gingival tissue. I have attached a full smile photograph this week to illustrate the extent of the grey shadow that is seen in her smile.
The idea of orthodontic eruption is an excellent one except for the tapered shape of the root, which may leave the patient with mobility post treatment. The option of crown lengthening a single central incisor in the aesthetic zone can lead to compromised papilla and an uneven gingival architecture. If the patient was planning to restore the remaining anterior teeth, crown lengthening the 4 incisors could lead to a more even result but we are still left with the dark color and low value of the remaining root structure for this central incisor.
With this in mind the patient decided to have a dental implant placed to replace this structurally compromised tooth. With the final restorative option decided we needed to determine how we would execute the treatment. There are 3 basic options when you are planning to replace a compromised anterior tooth with a dental implant.
1) Extract the tooth and place an immediate implant and graft the remaining socket.
2) Extract the tooth and graft the socket with a delayed implant placement at 3 months.
3) Extract the tooth without grafting the socket followed by an early implant placement at 6 weeks.
The next decision that needs to be made is about the form of provisional that you will provide for the patient. The different types of provisional restorations that can be created for a situation like this are:
1) Single tooth RPD or flipper.
2) Essix type of retainer with a prosthetic tooth.
3) Bonded Maryland type bridge.
4) Bonded tooth or crown to the adjacent teeth.
5) Immediate implant crown provisional.
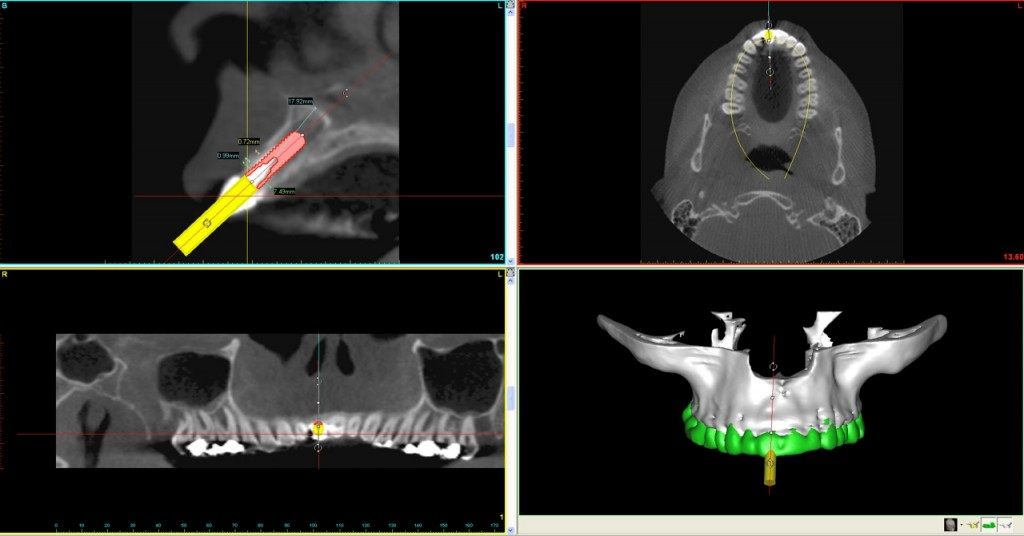
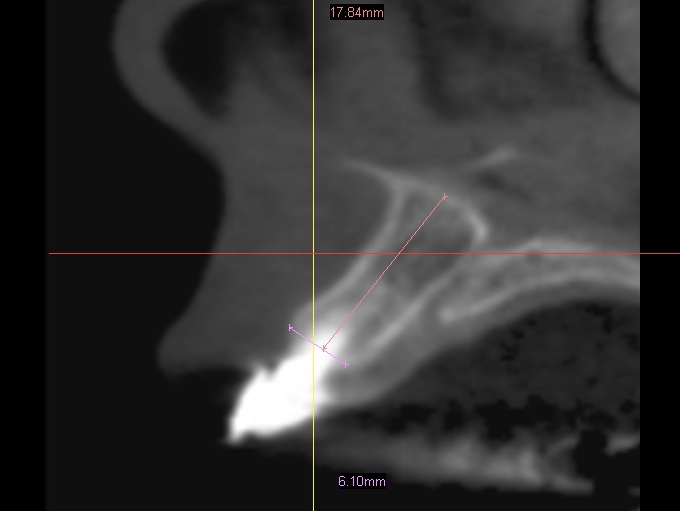
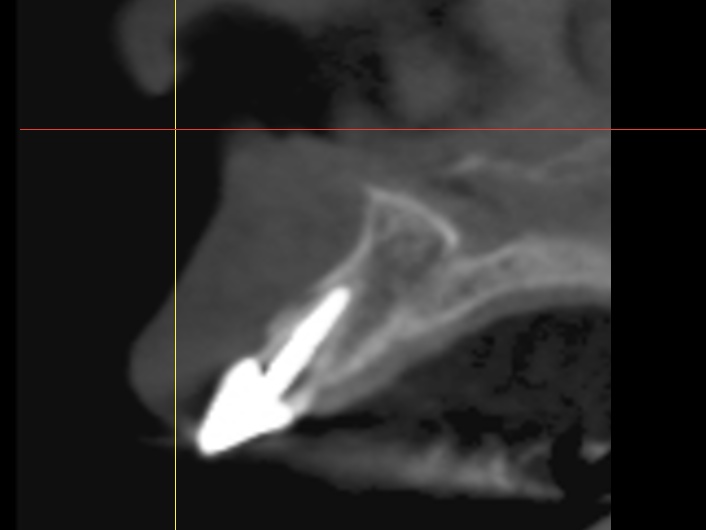
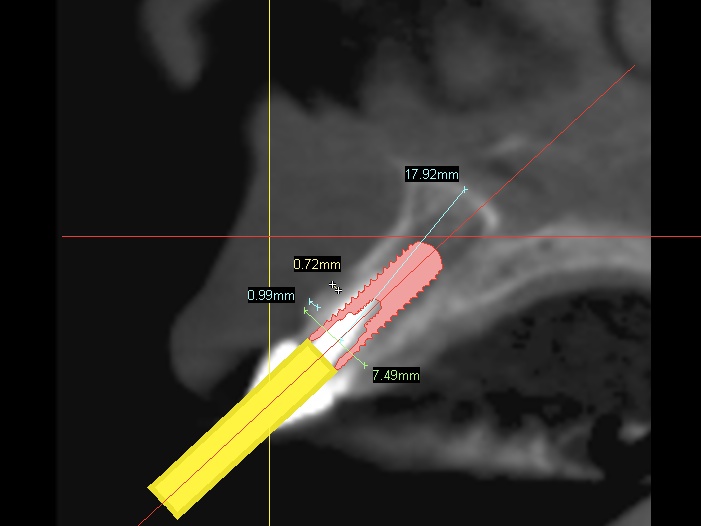
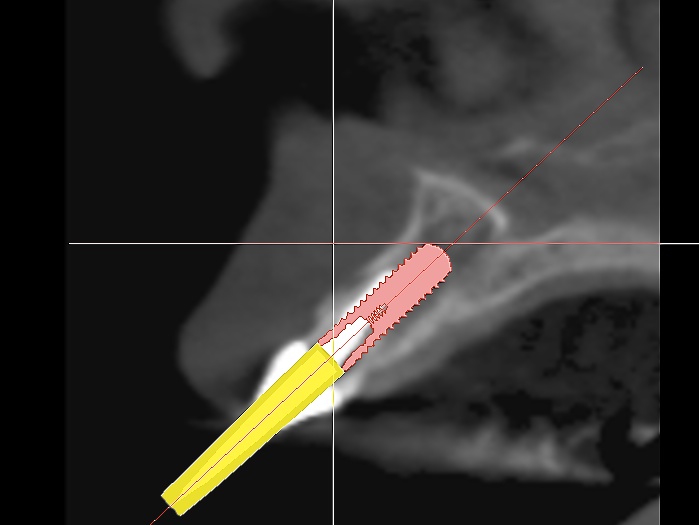
In this particular case we decided to have a CBVT scan completed to determine the thickness of the buccal plate and ridge volume and see if an immediate implant at the time of extraction is a reasonable treatment. If you look at the slices from the scan you can see that the patient has adequate height and width to the ridge but does she have enough thickness on the buccal plate. It looks like the thickness is less then 1.0 mm in the coronal half of the root.
To continue the conversation this week I would like to know what implant placement option and what form of provisional would you choose for this patient.
I would also like to know if the remaining buccal plate would factor into you’re the timing of your implant placement. As usual you can leave your treatment choice and comments using the link above this post.
Next week I will share with you more information about the treatment the patient has received for this case.
Post comments (19)
© Copyright Phelan Dental Seminars I Dr. Stephen Phelan





Nelly on June 29, 2017
If the buccal plate is in reality 1-1.5 mm and able to preserve it with atramatic extraction, possible to place immediate implant with delayed temporization and loading and placed buccal bone graft, preferably with PRF. Someone mentioned fiberglass temp, I also prefer something like that with ribbond to place ovate pontic if occlusion allows, or the other option (not sure why nobody mentioned) snap-on smile style temp – you can do ovate pontics and adjust them, looks great, no pressure on buccal bone graft, and I use it all the time for cosmetic implant temps. you can shape gingiva with it almost as good as with implant temp. And one can do gingival grafting etc having this temp easily
Ashmam on March 30, 2013
Very challenging clinical situation indeed…look carefully at the gingival biotype. Obviously with all procedures done over the years, we do expect some attachment loss…then CBCT view shows to the best 1-1.5mm buccal bone…again very challenging as Dr. Gary Ford mentioned in his observation.
I would definitely recommend the following:
1. A traumatic extraction
2. Thorough curettage both mechanically and then with Chlorhexidine irrigation
3. Use of Hard tissue Laser like Waterlase MD to Debride the area and de toxify ( if available)
4. Socket grafting with GBR
5. Delayed Implant placement
6. My feeling is that we would still need a connective tissue graft at 2 nd stage to improve pink esthetics.
Open for discussion!
Carlos Boudet, on March 30, 2013
Forced orthodontic eruption would only be of benefit if the gingival line were higher that the adjacent central or if you anticipated some tissue loss after implant placement and wanted to start with more tissue to begin with, and the patient is willing to put up with the longer treatment time.
Delayed implant placement will likely result in a deficient site at the labial, as the most remodeling occurs during the first 3 months after an extraction.
The most predictable results for bone and papilla preservation will be with immediate placement and temporization (in the right hands) or immediate delayed placement in 4 to 6 weeks.
The surgeon needs to do an atraumatic periotome extraction to avoid any damage or pressure to the labial plate.
A flipper is contraindicated in this case, as it would result in pressure against the ridge and tissue loss. The correct way to temporize with a removable is with an Essix with an ovate surface to help shape the tissues and keep the papilla, or even better a temporary tooth bonded to the adjacent teeth.
Javier Ochoa on November 25, 2012
Excelentes comentarios de todos se aprende. Lo mas importante es al momento de la extraccion,la cantidad de hueso remanente y si no esta danada la tabla se puede colocar el implante de 3.75 dirigido hacia palatino lo mas posible, regenerar y si la estabilidad primaria es suficiente colocar el provisional fuera de oclusion para conservar la arquitectura gingival.Si no se puede colocar el implante regenerar y poner un provisional de composit adherido con el pontico de forma ovoide, esperar 3 meses y colocar el implante con provisional y esperar el tiempo necesario para observar si es necesario hacer una remodelacion gingival antes de la toma de impresion definitiva
Dr Stephen Phelan on December 15, 2012
Thanks Javier!
Hayk on July 28, 2012
Hi
immediate implant placement (3.75 with maximal length, palatal position) existing gap and buccal plate grafting, immediate provisionalisation with gingival contour management, early or conventional loading.
Dr Stephen Phelan on August 4, 2012
Hi Hayk,
That is a great treatment plan. I would be a little cautious because I think you need to be very careful about the implant position to make sure you will not develop facial recession. The ideal of using a smaller diameter implant will help with this when it is placed in a more palatal position.
Regards,
Stephen
Galina Mayer on July 25, 2012
I didn’t realize this is a 2011 case 🙂
Dr Stephen Phelan on August 4, 2012
Hi Galina,
Yes it is a case and blog series that I produced last year. I wanted to send it out to all the new dentists on my email list because everyone liked the case so much when I sent it out originally. 🙂
I am glad you like it.
Regards,
Stephen
Natalia on July 25, 2012
In this case I would extract the root saving the alveolar bone as much as possible and graft the socket with a delayed implant placement at 3-6 months. To achieve a perfect aesthetics in the gingival part, I would make a fiberglassed bonded restoration of the missing tooth with a convexity in the upper part which will assure a perfect gingival edge for the new crown.
Dr Stephen Phelan on August 4, 2012
Hi Natalia,
Great comments and if you look at my next post you will see I agreed with your treatment recommendations.
Regards,
Stephen
Hesham Morsi on September 13, 2011
According to the cone beam views i think an immediate implant with a bone graft and delayed loading woulf greatly increases chances of success in this region considering the condition f the buccal bone. Implant width i recommend a 4,2 ~ 4,7
Dr. Gary S. Ford on May 27, 2011
What an awesome case and come back all I said previously. First off, lets look at the radiograph again, with the tooth, P&C, crown in place and consider that the post not only perforated the root but possibly, most likely, caused a fistula on the buccal plate. It would be interesting to do the surgery to remove this root and truly see how much buccal plate is actually there. So forget about immediate placement – graft and leave it alone for at least 4 months – I usually go 6 months. Provisionalization – either way, but you really need to keep the gingival form with an ovate pontic into the socket. I would keep my local periodontist on call to guard against the dreaded “black triangle” syndrome. I whole heartedly agree with photos, diagnostic wax up, and serious discussions about her expectations. Get her into a bruxism appliance soonest and good luck.
Syd on May 26, 2011
1mm bone on buccal… I always like to see 1.5 to 2mm at least. (I know that that is rare anyways)
So delayed placement of the implant would lower the risks a bit because its little unpredictable where that buccal plate will be when it heals. Early Delayed meaning 6wks. then graft if necessary.
If other teeth are to be restored a fixed option with a ponitc .
Or Temp abutment with pontic to contour the soft tissue during heaing. NO function of course.
Bruce Burgess on May 26, 2011
If I were doing the surgery, I think I would want to do a delayed placement. I would extract, do socket preservation with your favorite material and temporize. I would go in later, once the bone has consolidated, and bias the implant towards the palatal as much as I could get away with. This will help you with the gingival contour and colour. Depth of the implant head will be crucial. You might give yourself a bit more control of the aesthetics with a bone level implant. In any case I think some aesthetic gingivectomy / crown lengthening would be required prior to final restoration.
I normally temporize these with a flipper partial, but my oral surgeon buddy swears by Essix type temporaries. I think an Essex would be easier for me but not as nice for the patient.
I presume you are thinking about placing veneers and not crowns on the other teeth.
In a perfect world, I would love it if this patient went through ortho prior to the restorative phase. It would be nice to take all the occlusal issues out of play. It would make the restorative phase easier, more predictable, and have a better prognosis. It would also look better, possibly the only part the patient would hear. I explain this to all my occlusal patients, but only a few take my advice.
Nice case. Lots of ways to go that will lead to a great result for the patient.
Cheers.
rick on May 26, 2011
I like the thoughts of both of the above, as they show both logical thought, but varied approaches nonetheless. Somewhere in there it appears that the extraction/immediate implant route might not be a bad one, considering the possible placement of the implant in a more palatal position than that of the natural root.
In that case, the issue with the buccal plate might be lessened, with space for grafting material in that area increasing.
Then the issue of temporization. Since the bone is adequate except for the thin buccal plate, the implant may or may not be stable enough to support an immediate temporary, and that option could only be determined during the implant placement, so it would be a good idea to have a provisional ready just in case. On the other hand, it may turn out that it is best to leave the implant be with no forces on it until after a healing period has taken place. I am not a fan of bonded bridges to teeth which will not be involved in restorations, but in this case since the adjacent teeth will be receiving restorations (presumably crowns), I lean towards that option for patient comfort and to have no forces at all on the implant.
Joe Bulger on May 26, 2011
With her fairly high smile line, this becomes a challenging aesthetic case. Preserving the gingival architecture becomes a high priority, so I would lean towards the immediate implant and temporization route.
That compromised buccal plate becomes a factor in inserting the implant, but shouldn’t eliminate the opportunity for immediate placement.
About her smile, is the upper lip lifting asymmetrical, or is it the occlusal plane tilted, or a little of both?
The fortunate thing about this case is it looks like she has gingiva to spare on #12 and 11.
Joe 😀
Vaughan Glover on May 26, 2011
Obviously concerned about aesthetics and wants optimal long term function and aesthetics. No-one can guarantee the healing process with grafting thus immediate implant is not advised. Waiting a few months to have optimal long term contours and aesthetics just makes sense.
Since she is restoring the other anteriors I would suggest the following.
a/ diagnostic wax up using photos and possibly bonding the existing anteriors to establish optimal crown length aesthetics and phonetics.
b/Prepare the anterior teeth and make provisionals with optimal aesthetics and contours and making the 1.2-2.1 as a bridge. This type of a fixed provisional is much better than a flipper for a possible extended healing time.
c/ refer to have the 1.1 extracted and graft the site and allow 3 months for healing. With a questionable buccal plate, the delayed placement of the implant makes sense.
d/ After appropriate healing, place the implant using a stent to guide the surgeon.
e/ during healing the gingival contours can be assessed and if necessary do crown lengthening or contouring.
f/ after whatever healing time is required we should then be able to predictably proceed with long term porcelain restorations while managing the tissues for optimal contours and emergence profile.
g/ Regardless of how much time is allowed for healing, the client should be clear about the fact that future adjustments or even re-treatment of the restorations may by necessary as changes in tissues and contours can happen. The implant itself is permanent and thus it is essential to take all the time required to ensure it is in an optimal position.
Donna Brode on May 26, 2011
Great pictures! The gold standard has changed.