- Home
- keyboard_arrow_right Phelan Dental Seminars
- keyboard_arrow_right Part 3: Would you extract this tooth or not?

Hi everyone, once again I would like to start off by thanking all of you for the excellent ideas and comments related to last weeks post.
Today I would like to share with you how I handled the extraction, socket grafting and provisional issues that this case presented with, but first I would like to address the question about immediate or delayed implant placement.
As you could see by the CBVT images the buccal plate was fairly thin in the coronal half of the ridge with volume of less then 1.0 mm thickness. I spent a week at IDEA in San Francisco 2 years ago at a course presented by Dr. Dennis Tarnow about aesthetic implant techniques and he taught us if in doubt to follow the principle of doing one miracle at a time.
With this in mind if the buccal plate is missing or very thin the most predictable treatment option is a delayed implant placement. In this particular case we started out with excellent gingival architecture and a fairly high smile line so I wanted to design the treatment strategy to preserve and protect the pretreatment contours.
The 2 options if you are considering a delayed implant placement are to extract the tooth and not graft the site followed by an early implant placement at 6 weeks. This is the technique advocated by Dr. Danny Buser and he generally preforms a contour augmentation of the ridge at the time of the implant placement with a GBR technique.
The second option is to remove the tooth, graft the socket and support the soft tissue profile with the provisional restoration. This is followed with the implant placement at 3 months using a minimally invasive surgical technique.
In this case because the tissue architecture was ideal before the extraction I decided to follow the second option because if you remove the tooth without grafting and soft tissue support you loose most of your ideal tissue architecture. The overall tissue architecture then needs to be rebuilt with the GBR technique and later with the implant provisional. I believe the first option with the GBR technique is best utilized when the patient starts out with less than ideal tissue architecture that will need to be rebuilt regardless if you graft the socket or not.
My point with all of this is that if you have excellent tissue contours before the treatment starts you need to plan your therapy to preserve these contours with your treatment strategy.
For this case I started by extracting the tooth using a periotome elevator and an atramatic technique. One of the most important concepts you need to keep in mind is that you cannot raise a flap to remove these teeth and expect to maintain the tissue architecture. If you raise a flap to extract the tooth you are going to loose most of the soft tissue architecture and likely the buccal plate of bone.
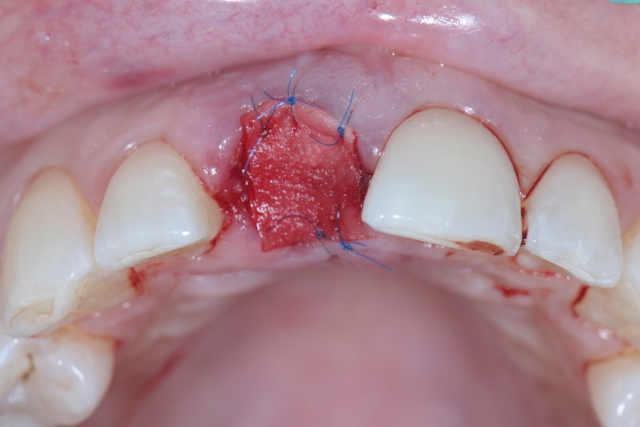
In this case I did my best to remove the tooth without surrounding trauma and then I accessed the socket. The buccal plate was intact but appeared fairly thin so I grafted the socket with Puros cancellous particulate allograft and placed a BioMend Extend barrier membrane and sutured the membrane into place with 6-0 polypropylene monofilament sutures.
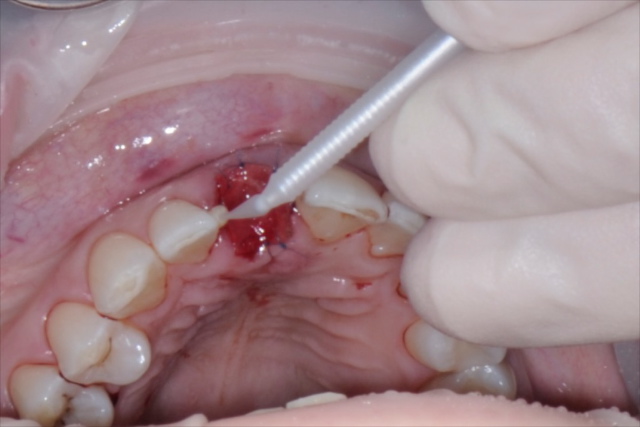
To create a provisional restoration that would support the soft tissue architecture I cut the old crown from the tooth and bonded the endo access that would face the ridge with composite resin.
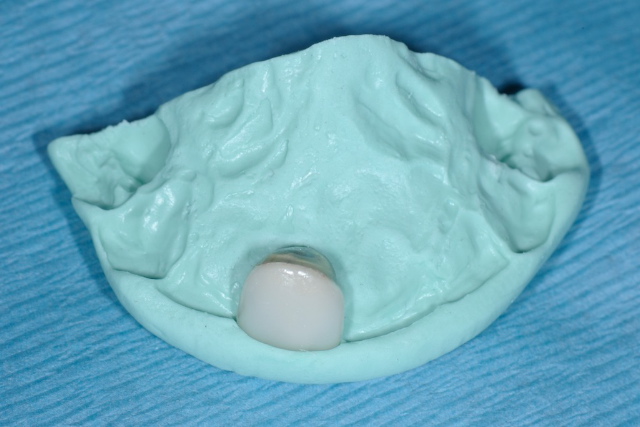
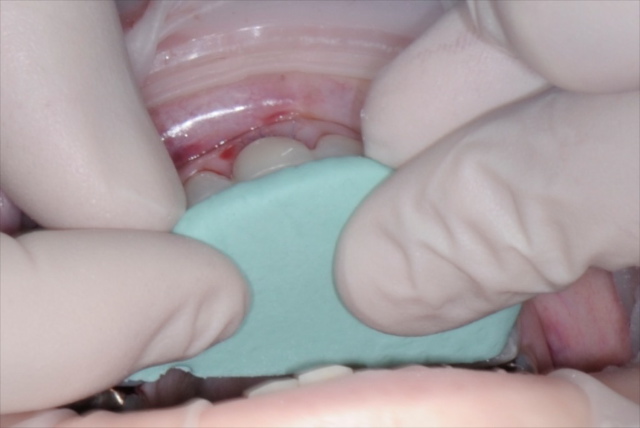
The next step was to attach the crown to the adjacent teeth and this patient has a deep overbite so I decided to bond the crown to the proximal contacts of the adjacent teeth. To facilitate the placement of the crown in the correct location I made an Incisal putty matrix on the pretreatment study model. I placed the adjusted crown into the correct location on the putty matrix and boded it to the adjacent teeth using Optibond adhesive and flowable composite.
As you can see by the photos I have included from this case the overall tissue architecture has been effectively preserved using this protocol.
To continue the conversation this week I would like to know if you would raise a flap to place the implant and if you would place an immediate provisional.
Graft and Membrane Sutured Into Place
Preparing to Bond the Provisional Crown
Provisional Crown in the Putty Matrix
Provisional Crown Bonded into Place
One Week Post Surgery After Suture Removal
Final Implant Site Development
Post comments (46)
© Copyright Phelan Dental Seminars I Dr. Stephen Phelan










Elie Warde on December 15, 2017
Hello Stephen. If you have to treat this case today (in 2017 ) would you plan for an immediate implant using partial extraction technique PET socket sheild technique with an immediate temporary crown ? Thank you for sharing interesting and delicate issue
Regards. Elie
richard leekin on April 15, 2013
Dear stephen ,
beautiful soft tissue mangement, would you have considered using some Connective tissue graft instead of membrane here ?
thanks
………………
richard
saurav on April 14, 2013
thanks for the blog doc…. learning a lot from you … nice case
Marshall S Dicker DMD FAGD on April 13, 2013
wasnt it Dr Tarnow who also said
” no tickee…..no shirtee “???
little humor there
Marshall S Dicker DMD FAGD on April 13, 2013
I had a case very similar to this one…….only due to previous perio problems……..there was no buccal bone.
The O/S removed the tooth and placed graft material with the provision of MORE grafting at a later time
The patient had old all porc crowns on either side of the tooth to be removed.
i fabricated a flipper temp, which the patient broke about 6 weeks later and i repaired it.
since there were 2 old crowns on either side and the O/S agreed enuf of the bone graft he
placed had converted ( not enuf for an implant tho ) we started the bridge.
i think either a thin or absent buccal plate is SUPER important, IF an implant will be used.
Dr Stephen Phelan on April 13, 2013
Yes, Great comment! As Dr. Dennis Tarnow told me, “No buccal plate, No implant”
Marilyn K Jones DDS on April 13, 2013
Great Case. Wonderful Photos. Thanks for sharing.
Dr Stephen Phelan on April 13, 2013
Thank you I am glad you like the case!
Patti-Anne on December 7, 2012
Hi Steve,
This post has been so useful for me. I can’t tell you how many times I have come across a similar situation and struggled with how to best manage the case. Just wondering if you can share some tips and the instrumentation you utilize for removing such compromised teeth (anterior and posterior) without raising a flap or removing bone. Even when I send cases to oral surgeons for extraction and socket preservation, with the intention of having an implant placed, the surgeon often ends up removing bone leaving the patient with an unfortunate defect in the area.
Thanks,
Patti-Anne
Dr Stephen Phelan on December 15, 2012
Hi Patti-Anne,
I am glad you are enjoying the blog. You really want to try and avoid raising a flap if you want to preserve the papilla and ridge in the anterior region. If you look at the comment above by Chris the Benex root extractor system works really well with intact roots but the kit is really expensive. I generally use a series of periotome elevators. I have a kit that I ordered from Salvin that works really well.
Regards,
Stephen
ELIE on December 1, 2012
Hi Stephen,
Nice case. i Followed the case on your Facebook page.
Well done
Regards, Elie
Dr Stephen Phelan on December 15, 2012
Thanks Elie!
Chris Barlow on December 1, 2012
Hi Stephen,
Yes, I would also use a Cytoplast PTFE membrane.
Nice end result. As you know, preserving the integrity of the papillae is important in order to preserve the supporting underlying bone. Have you ever tried, or seen, a Benex extractor which literally pulls the root straight out of the socket for atraumatic extraction?
Dr Stephen Phelan on December 15, 2012
Hi Chris,
I have that Benex root extractor system and it works really well as long as the root is intact with minimal caries.
I may create a post about that system in the future. I would like to video tape it at some point.
Regards,
Stephen
ELIE on November 4, 2012
We never leave a collagen membrane exposed, better to use a PTFE membrane for 3 weeks ?
Dr Stephen Phelan on November 30, 2012
I am using the Cytoplast membrane now if the site is exposed but for this particular case the extraction socket and membrane were largely covered by the bonded pontic. I think the overall results are fairly good.
Hayk on August 2, 2012
Dear Stephen
Thank you for nice presentation, this helpful to thinking about different approaches one more time.
Let me ask: Would you choose other way for this situation in case ,for example, the patient would be able to visit for procedures only two multi visit times with 6 month Interval and expects to get permanent tooth in the end of second visit? (or to reduce visiting, surgery, may be cost)?
Thank you in advance.
Hayk
Dr Stephen Phelan on August 4, 2012
Hi Hayk,
I am not sure I could shorten the treatment for this case and keep it as an implant. I may be able to make it faster and with less visits with a fixed bridge.
Regards,
Stephen
Udi on August 1, 2012
Dear Dr Phelan
I’m happily joining all the complements for your newsletter.
I would not use a flap. I would use a CT to evaluate the results of the GBR and would place an implant in the most conservative way possible.
Udi
Dr Stephen Phelan on August 4, 2012
Hi Udi,
I totally agree with you as you will see with next weeks post!
Regards,
Stephen
Scott Bobbitt on August 1, 2012
Absolutely flap and immediate provisional! Great looking case so far. Thanks for the post
Dr Stephen Phelan on August 4, 2012
Hi Scott,
Did you mean flapless implant placement?
Regards,
Stephen
Bilgee Jigjid on August 1, 2012
Hi Dr. Phelan
Thank you for your nice and usefull case presentation. Here in Mongolia we also have many cases needed to be done very carefully in implant replacement area like this.
I have got some useful tips and I waiting for your next coaching in the next week.
I am enjoying all your posts and occlusion design trainings and rolling them again and again.
Thank you
Bilgee
Dr Stephen Phelan on August 4, 2012
Hi Bilgee,
Thanks for the comments! I am on a fishing trip in Northern British Columbia this week and I am planning for the next Occlusion Design Member coaching webinar for 2 weeks from now. You will receive an email in a week with the details.
Best regards,
Stephen
Nasser Emtyazi on July 31, 2012
Dear Dr.Stephan,
Thank you very much .I am waiting for next step.
regards
Dr Stephen Phelan on August 4, 2012
I am glad you are liking the series Nasser!
Regards,
Stephen
Galina Mayer on July 31, 2012
Excellent result, Stephen!
I am sure you built up the inside of the crown to extrude a bit up into the socket in order to build such a nice socket that we can see on the last two pictures.
Any plans for the occlusal repair on the upper front 6? What are the reasons for the wear? Is this a younger pt?
Thanks for sharing, I am sure pt. is already elated!
Dr Stephen Phelan on August 4, 2012
Hi Galina,
As you watch the series you will see what we developed for the occlusion. At the beginning of treatment I did a functional analysis and occlusal records then presented an ideal treatment plan.
Thanks for the comments, Stephen
Dir1 on June 6, 2011
Hi Dr Phelan
Great job. The CBVT images have been really helpful. I am looking forward to the next blog about the implant placement.
I want to suggest Dentist delhi , a Delhi based dental clinic , may be helpful to you.
Dr Stephen Phelan on June 7, 2011
Thank you and I checked out the website, it looked great!
Thanh Nguyen on June 6, 2011
Hi Dr. Phelan, I am thinking about another way, if I got the tooth out without surrounding trauma, I could place the immediate implant ( for sure have to be placed toward the palatal wall), then tuck cancellous bone grafting material to the void between the implant and the buccal wall.
If the implant can be torque to 40 Ncm, I will make a temporary crown using composite on temporary abutment and crew to the implant to maintain the gingival contour. The provisional crown has to be out of funtion.
If I cannot torque to 40Ncm, then I will close it up with membrand and bond the crown to the adjacent teeth as well
Dr Stephen Phelan on June 7, 2011
Hi Thanh,
I think your treatment plan sounds great. I was concerned with the condition of the buccal plate so I decided not to place the implant but I likely could have placed it without any problems using the technique that you described. According to my training from Dr. Dennis Tarnow, I would not try and obtain immediate closure after grafting around the implant in an extraction socket.
Samir on June 5, 2011
))) sorry for “mucotom” ! i mean tissue punch !
Dr Stephen Phelan on June 7, 2011
Yes, I used a tissue punch. I will show that in this weeks blog post.
Dr Stephen Phelan on June 5, 2011
Samir,
I am not sure what mucotom is? I will show the implant placement technique next week.
Thanks for the excellent questions.
Stephen Phelab
Samir on June 5, 2011
one more question) during implant procedure did you use mucotom ? or made flap?
Samir on June 5, 2011
Hi Dr Phelan !!! Nice case !!! why dont you place implant immediately after extraction? Is biomend membrane resorbable?
Dr Stephen Phelan on June 5, 2011
Hi Samir,
The Biomend is a resorbable membrane and the reason I did not place the implant immediately is that the buccal plate was fairly thin and I was worried about mid-facial recession.
Louise chow on June 2, 2011
Great case and beautiful outcome! How did the crown stay in place with just interproximal flowable resin?
Dr Stephen Phelan on June 3, 2011
Hi Louise,
Thanks for your comments. The provisional crown stayed in place until the time that I placed the implant over 3 months later. I had to cut it off to remove it and I have used this technique a number of times with similar results.
Anoop on June 2, 2011
Great job Steve. very informative and detailed.
Given his deep bite, is a flowable bonded to porcelain crown strong enough to hold for the duration?
I am sure we all have had the challenge of repairing broken porcelain, only to have it fall off the next day.
Also, how do you control the possibility of contamination from the fresh extraction site?
Your insights would be appreciated.
Dr Stephen Phelan on June 3, 2011
Hi Anoop,
Thanks for the comments!
The provisional held up really well for over 3 months until I was ready to place the implant. I did adjust the provisional crown out of occlusion and shorten the incisal edge so that it was not contacting in protrusive.
For the porcelain surface I microetched, silanated with RelyX Ceramic Primer and bonded it with Optibond Fl adhesive.
The BioMend Extend membrane sutured into place seems to cut down on the bleeding from the extraction site a great deal so that it is usually not a big issue.
anisa on June 2, 2011
Superb : )
Q: how do u remove the provisional during implant placement ?
( is there a method to drill through the interdental flowable contacts )
And the answer to ur question:
Non flap implant placement approach followed by immediate provisional.
BTW: ur emails are very tech sensitive and a great help as they are full of helpful tips.
thanks.
Dr Stephen Phelan on June 3, 2011
Thanks Anisa,
I removed the provisional crown by cutting through the proximal contacts of the provisional with a thin diamond (KS0) and then polished the natural teeth carefully to remove the composite with Soflex XT discs and Enhance cups.
Joe Bulger on June 2, 2011
Fabulous results Stephen!
Dr Stephen Phelan on June 3, 2011
Thanks Joe, Next week I will show the implant placement.