- Home
- keyboard_arrow_right Phelan Dental Seminars
- keyboard_arrow_right Part 4: Would you extract this tooth or not?

Hi everyone, once again I would like to start off by thanking all of you for the excellent ideas and comments related to last weeks post and let you know that if I have not responded to your comments yet I will in the next week. It really is great to see everyone’s ideas about treating a case like this and I enjoy all of the comments and suggestions.
Today I would like to share with you how I handled the implant placement and provisional issues that this case presented with. As you know from last weeks post I elected to graft the socket and delay the implant placement for three months for the bone to heal and the soft tissue to mature around the provisional crown.
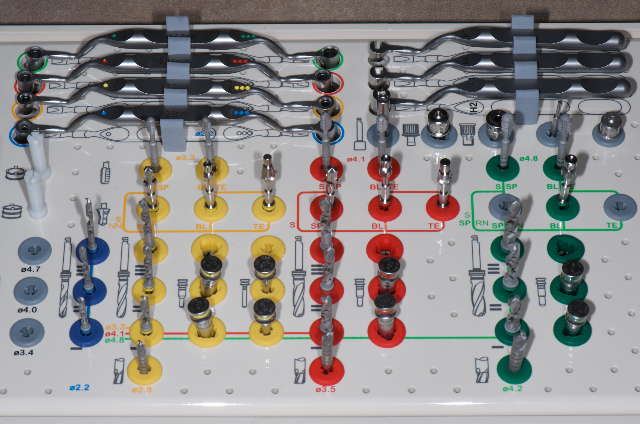
For the implant placement I had a Simplant Surgiguide made from CBVT scan of the case. The Surgiguide is a steriolithographic stent, which was constructed on the stone model of the patient’s mouth with the central incisor removed. This particular Surgiguide was made with a 5.0 mm Straumann sleeve that will guide the implant placement with depth control build into the system.
The first thing I needed to do was to remove the provisional crown that was bonded to the adjacent teeth. I did not want to damage the unprepared adjacent teeth so I used a thin Axis Dental KS0 cylinder diamond to cut through the old crown leaving a little of the flowable composite on the adjacent teeth. I then polished this composite with composite polishers and assessed the remaining ridge and the fit of the Surgiguide. As you can see by the photos I took after the provisional removal the ridge and soft tissue displayed excellent healing from the socket grafting procedures.
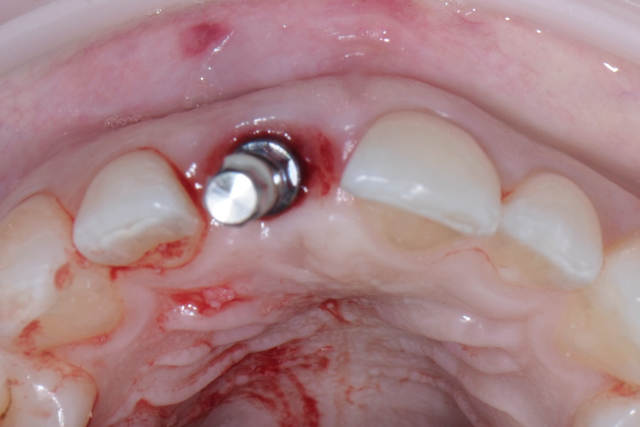
At this point the decision needs to be made if you flap or punch the tissue to place the implant. In this case because of the ridge preservation procedures the site does not need any contour augmentation and the soft tissue profile looks excellent. I also have a CBVT scan of the site and a Surgiguide to guide the implant placement so the most logical treatment approach is to punch the tissue and use the guide to drill the osteotomy.
I used a 4.0 mm rotary tissue punch through the Surgiguide to remove the soft tissue prior to drilling the osteotomy. As a general rule I remove the punched tissue with a scaler and save it in a sterile bowl with saline in case I need it for contour augmentati
on after the implant placement. With this patient the tissue was not needed due to the preservation of the soft tissues with the grafting technique.
I proceeded to prepare the osteotomy using the Surgiguide and the Straumann Guided Surgery Kit, taking a radiograph after the initial 2.2 mm and the final 3.5 mm twist drills to confirm the location, angulation and depth of the osteotomy.
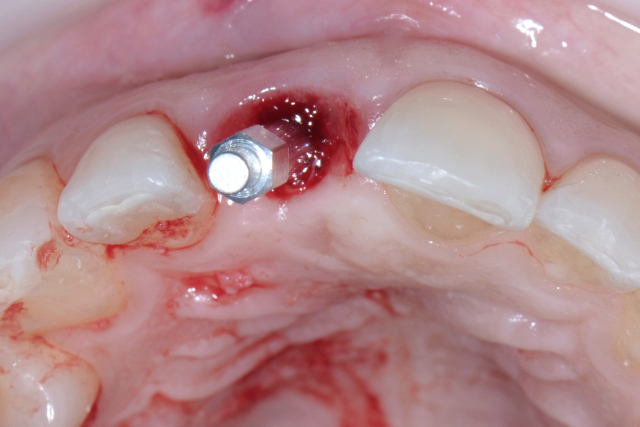
The implant, a 4.1 mm RC Bone level implant was placed to a depth of 3.0 mm below the CEJ of the adjacent central incisor. I used the adjacent central incisor because the grafting technique left the free gingival margin of the implant site slightly coronal to the natural central incisor. I then tested the stability of the implant with the Osstell system and the ISQ measurement indicated that the implant had excellent primary stability and should be suitable to place an immediate provisional.
The next step was to create a screw retained immediate provisional with fairly flat contours and emergence profile to avoid placing too much pressure on the soft tissue at the surgical site. I adjusted the provisional so it did not contact in centric and shortened the Incisal edge so that it would not contact in protrusive.
The patient has now completed healing after the implant placement and it appears that we have excessive tissue at the free gingival margin. This is a good problem to have but I would like to know what all of you would do to complete the treatment of this case. Would you remove the excessive tissue with a laser or push it apically by adjusting the contours of the provisional implant crown? We will also need to consider the Incisal wear and provide the patient with some form of protective appliance.
Please let me know If you have enjoyed this blog series, and also if you have any suggestions for future blog topics because I would appreciate the feedback.
If you would like to really boost the fun and profitability in your dental practice you should consider learning more about guided dental implant surgery. Take a look at my new seminar Interdisciplinary Aesthetics for Implants and Teeth hosted at the Niagara Fallsview Casino and Resort on Sept 30th and Oct 1st, 2011. You can click on the link here to learn more about this entirely new seminar.
Final Implant Site Development
Final Implant Site Development
Surgiguide
Straumann Guided Surgery Kit
Implant Site Tissue Punch
Implant Placed into the Tissue Punch
Osstell Placed on Implant
Testing the ISQ with the Osstell
Adjusting the Meso Provisional Abutment
Completed Provisional Abutment
Completed Provisional Labial View
Completed Provisional with Flat Emergence Profile
Completed Provisional Palatal View
Before Treatment
Implant Provisional in Place
Post comments (18)
© Copyright Phelan Dental Seminars I Dr. Stephen Phelan















Julian Caplan on December 8, 2012
Dear Stephen,
Well done on a fabulous series. You follow well defined logical steps with an element of group discussion which is a pleasure to read. The few negative comments that are made are to be expected – whenever you put your head above the parapet expect to be shot at! The standard of you dentistry is obvious and is inspirational.
Again congratulations and please keep them coming!
Regards,
Dr Julian Caplan
Dr Stephen Phelan on December 15, 2012
Thanks Julian,
I appreciate the feedback!
Regards,
Stephen
Alvin Matteson on August 9, 2012
Nice Case!!!, With the provisional did you under contoure the the soft tissue allowing the tissue to be contoured in lab to ideal or do you idealize the contours first? The ovate pontic site looks excellent.
Dr Stephen Phelan on August 21, 2012
Hi Alvin,
I actually idealized the contours of the provisional and tissue before I had the final restoration fabricated.
Regards,
Stephen
Omid on November 28, 2011
Hello Dr. Phelan,
Beautiful surgical pictures!
If I may ask, what is the name of the retraction device being used for this surgery, and who manufactures it?
It appears to be a hybrid of sorts using a rubber damn connected to a rigid extra-oral plastic ring?
Thank you in advance,
Omid Kiarash
Stephen Phelan on November 28, 2011
Hi Omid,
The retractor is an OptraGate from Ivoclar Vivadent. It is really a great retractor for anterior restorative.
Best regards,
Stephen Phelan
Jonathan on June 27, 2011
Hi Dr. Phelan
I want to say that I’m just amazed by the impeccable work here… I just graduate 5 months ago but now I’m sure that I want to make aesthetic dentistry.
Greetings from Venezuela
Stephen Phelan on November 28, 2011
Thank you!
syd on June 13, 2011
Stephen,
The case is looking great. I have been to some of your seminars and enjoyed them. I know there is a lot of things you do consider in the background such as occlusion and esthetics etc. Even so far as how far to sink the top of the head of that implant relative to adjacent teeth. Question: what was your decision process on the implant type and size? As for the excessive tissue… I might consider restoring it as is and waiting for the tissue response over the next 4-6wks then lase it off , if needed.
Vaughan Glover on June 10, 2011
Stephen and all,
I would like to say that my initial response to the challenge you presented was not the way I would approach this case in my practise and when I view these photos, there is a high risk that this treatment is a failure for the person. It is beautiful technical dentistry, but could well be a wasted investment in her life plan. Let me explain.
I have never responded to an online discussion like this, so I answered the question you presented. However, my mission is not to fix teeth but to help people to be the best they can be.
This well may be a failure, not because of the excellent result with grafting, surgical technique, provisional and the restoration.
THis is a failure because everything MAY be in the wrong position. Your treatment plan and this discussion is about treating a tooth and not the person, the whole mouth, supporting structures and masticatory system.
Rushing ahead and fixing teeth is a critical mistake in our profession, as more and more people are doing implants.Your final comment was “We will also need to consider the Incisal wear and provide the patient with some form of protective appliance.” I suggest that this is wrong.
The very first thing I would do is a comprehensive exam and workup. One piece of this exam, would be to do an occlusal evaluation, assess centric and figure out why the incisors look the way they do and perhaps discuss the fact that if I put porcelain on one tooth and this habit or parafunction continues, that within a year, the only tooth that will be in function will be the implant.
When I see that type of wear on the anteriors then something is wrong and must be dealt with before we rush in and fix teeth.
I did mention I would do a diagnostic wax up and I believe it is critical in a case like this. I would have her bring in photos and show her the difference between the way her teeth are now and the way they were before wear and ask what she wants to look like for the rest of her life. This discussion must occur before people invest $5,000 or more in one tooth.
I believe this is a critical oversite that could and likely will drastically change the treatment plan. She may need ortho, or splint therapy to establish centric, or equilibration or ??? I have no idea, but it must be decided before we start fixing.
She may or may not choose to restore the other anteriors. That is her decision. The important part is that she understand her options and make decisions before doing irreversible dentistry.
Personally I suspect that she is not in centric and has posterior slides. Regardless of what it is, this needs to be dealt with before we decide how to fix a tooth.
I was in a meeting recently where a prominent dentist stated that “too many dentists are into the business rather than the profession of dentistry”. Rushing ahead and placing implants and fixing teeth with an irreversible, integrated implant, is something that we must think about.
I am reminded of a comment by Pete Dawson and Alvin Filastre: “Above all else, avoid doing single tooth dentistry.”
I welcome your thoughts on this.
All the best.
Vaughan
Dr Stephen Phelan on June 10, 2011
Vaughan,
I appreciate your feedback and I have not checked with my records but I would need to assume that you have not attended one of my seminars. If you had attended one of my seminars in the last few years you would not assume that this is a failure because I did not treatment plan the case and decided to focus on single tooth dentistry!
I have a system I follow based on my training with Kois, Spear and Dawson and all of these patients first have a functional analysis with centric relation mounted models, examination and digital photo series. I then have a treatment planning consultation before any treatment is initiated.
This patient had this evaluation and consultation before the tooth was removed and decided not to have porcelain veneers to restore the wear on the remaining anterior teeth.
The treatment plan does include some strategic bonding to improve the anterior guidance and an equilibration prior to the final implant crown fabrication and an E splint appliance after the restorative treatment is complete.
I appreciate your feedback and all of your points make sense but this was intended to illustrate how to manage a specific situation and not a course about comprehensive dentistry. If you speak to anyone that has attended my seminars you will find out I am not about “doing single tooth dentistry”
best regards,
Stephen Phelan
Galina Mayer on August 7, 2012
NOW IT ALL MAKE SENSE!
Vaughan, you are absolutely right – this is not one tooth dentistry, this is full mouth dentistry. Well said!
Stephen is a ‘comprehensive dentistry’ professional, and he had an amazing seminar on thorough assessment, evaluation, diagnosis and treatment planning. So I knew that there was a serious tx. plan, and I was sure everything was explained to the pt. time and time again. I guessed that the pt. did not accept the whole tx. plan, and they will have to accept consequences. Would you agree that STRATEGIC BONDING, EQUILIBRATION AND E-SPLINT make total sense given the circumstances?
Galina Mayer on April 23, 2013
Gerald
You are absolutely right! I am sure it is as frustrating to Stephen as it is to you when you recommend an excellent treatment plan to the pt., but they won’t or can’t go ahead with it and so you have to compromise. Stephen would have been ecstatic if the pt.would accept his tx. plan recommendations in full. But…
When pt. loses the front tooth and you are only given an OK for this one tooth to fix, you don’t have much choice but to do what Stephen did: thorough exam and evaluation of occlusion, tx. planning and presentation to the pt. I know that Stephen explain to the pt. the consequences of the option that the pt. have chosen and pt’s liability should things go wrong.
Maybe Stephen can expand on how he handled the worn occlusion – given the circumstances – both prior to final implant crown fabrication and after the restorative tx was completed.
Thanks
Sean Harris on June 30, 2017
Love it. Some people should do their research before being critical.
Joe Bulger on June 9, 2011
Terrific set of photos to display your steps for the temp, and a very pleasing aesthetic result.
I really enjoyed this 4 part series. You opened things up with general discussion on treatment decisions and then gradually walked us through this case. Probably the most engaging and informative blog series I’ve ever seen.
Well done Stephen. You’ve raised the bar for our profession.
Joe 😀
Dr Stephen Phelan on June 10, 2011
Joe,
Thanks so much for the positive feedback. I really appreciate it!
Cheers, Stephen
Anoop Sayal on June 9, 2011
Hi Steve,
Nice detail and description. where do you send your patients for their CBVT imaging?
what would you charge this patient in this case?
If it’s okay with you, I would like to shadow you in your office for a few hours. Let me know if it is okay with you and we can work out time/day. you can email me directly at drsayal@georgetowndental.com.
Regards,
Anoop
Dr Stephen Phelan on June 10, 2011
Hi Anoop,
I use a new radiologist in Mississauga for the imaging. You can get the contact information from my office if you want to call them or ask Melissa.
I will try and send you an email in the next few days.
Regards,
Stephen