- Home
- keyboard_arrow_right Phelan Dental Seminars
- keyboard_arrow_right Would you extract this tooth or not?

I wanted to share with you a case that presented to my office a few months ago and see what your opinion would be about the best approach for treatment.
With this case the patient presented with a central incisor that had previously been treated with an endo, post, core build-up and crown. The problem was that something was loose. In this particular case the margins were not supragingival so it was hard to tell what exactly was loose!
In a case like this, either the entire tooth, post core and crown is loose or the post core and crown is loose, or maybe just the crown is loose.
I really could not tell during the emergency visit so I decided to reappoint the patient a few days later when I had more time to assess the situation and provide some form of treatment.
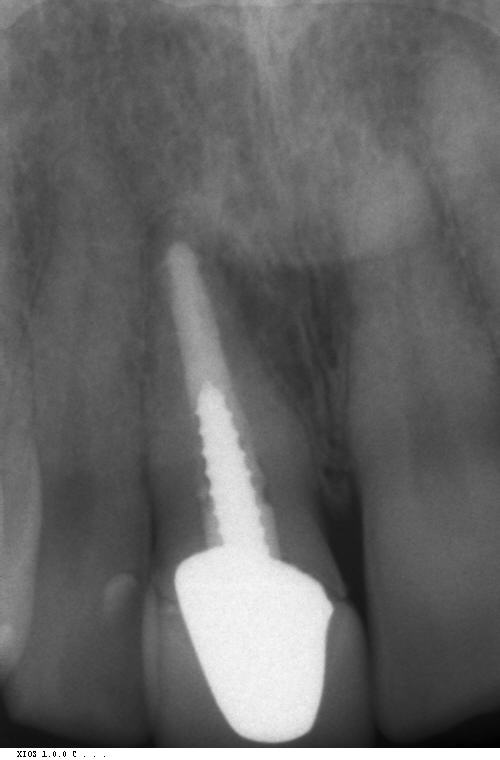
At the next appointment I tried to remove the crown and the post, core, and crown came out in one piece. You can see by the photo that there is not very much remaining tooth structure and minimal ferrule. The remaining root has a small amount of recurrent decay but no mobility and normal periodontal architecture.
I provided the patient the following options for treatment:
- Remove the remaining root, graft and place an immediate implant.
- Remove the remaining root, graft the socket and plan to place an implant 3 months later.
- Remove the remaining root, graft the socket and prepare the adjacent teeth for a fixed bridge
- Remove the remaining root and prepare the adjacent teeth for a fixed bridge without grafting the socket
- Remove the remaining root and place an RPD.
- Recement the post, core, and crown
- Crown lengthening surgery followed by a new post, core and crown
As you can imagine giving the patient a list of options like this is important for informed consent but can lead to confusion for the patient to make a decision.
In a case like this the patient will inevitable ask you what you would recommend for the treatment if this were your tooth.
What I would like to know is how you would treat this patient. I gave the patient 7 options for treatment and I would like to find out your treatment recommendation if this was your patient. You can leave your treatment choice and comments using the link above this post.
Next week I will share with you the treatment the patient has received for this case.
Post comments (182)
© Copyright Phelan Dental Seminars I Dr. Stephen Phelan






Baigalmaa on December 3, 2016
I will suggest option 2 and 7 from your list.
DR A. S. AL AMRO on December 3, 2016
Dear
Thanks for sharing these cases with us
2 option :-
1 extrusion, new casted post and core and crown
2 delayed immediate implant , implant after 6 to 8 weeks from extraction
Swati on December 3, 2016
I will prefer extraction and then graft followed by immediate implant/implant after 3 month.
Amal on December 3, 2016
I would go with the implant replacement after three months
Bruce Deckler DMD on December 2, 2016
Of course carefull extraction graft and place implant is the best solution with a flipper for at least 3-4 months. or extract graft , flipper and later implant. There does appear to be decay in the canal. Nice ferrule maybe extrude and cast post but there appears to be a more difficult preditable out come with implant.
Tilal on December 2, 2016
According to the remaining tooth structure keeping the root is not a good idea because crown length might end up with high gingingival line and poor esthatic so the extraction and immediate bone graft and implant the my treatment choice here.
HY on November 30, 2016
Is the fracture at or coronal to the base of the sulcus? If yes, I would not necessarily do a crown lengthening. I would prep for a cast post – but the prep would have to be tapered in a “V” shape so that the post compresses the root to lessen the risk of a root fracture.
If the fracture is apical to the attached tissue, the biologic width will be violated and then a crown lengthening will be needed.
Patient would be informed that there is some risk of fracture. If the risk is not acceptable to the patient, I would opt for #2 – extract, graft implant. NOT immediate loading. Looks like the patient is a bruxer – there are facets on the incisal edges, so immediate loading would be risky.
JR on November 29, 2016
I have successfully restored teeth in this condition. Some crown lengthening could be accomplished, and actually
improve the gingival symmetry. It looks as though a couple mm’s could be picked-up interproximally for an improved
ferrule, without encroaching on the biologic width. This would have to be done judiciously to maintain as much bone as possible, and with the unfavorable root form in mind. post, and core and of course crown would be redone. The only real downside is losing potential bone for an implant if it were required in the future.
I would let the patient know this would be somewhat “heroic”, and if they had no tolerance for that I would extract the
tooth, place an immediate implant with a graft, and a duraflex temp.. The biotype of this patients gingiva I think would lend itself to implant tx./graft without a untoward reaction, or recession of tissue.
Saud on November 29, 2016
Hi,
I would stay away from fixed conventional bridge as the adjacent teeth are sound and healthy as this would compromise the pupal health so I would go for adhesive single cantilever rather than conventional. If this was my tooth would recommend minimal invasive treatment 1st which is Ortho extrusion of root and new post/core/crown. In worse case senario ,extraction / immediate lmplant placement with no loading/ temp resin retained bridge / restoration and loading after 3 months
Bruce Deckler DMD on December 2, 2016
I like this Idea looks reasonable and promising
Tracy on November 27, 2016
Having dealt with this situation before more than once, I would plan for the extraction/graft/implant. Recement for now, address the lower anterior occlusion via ortho to get those labially tipped crowded incisors in alignment. Then revisit the implant. The majority of the time when these incisors start failing there is an occlusion issue. If it’s not addressed, as you know, we end up with buccal plate and/or fractures. I don’t want the same occlusal forces on my implant.
Noor on November 27, 2016
Hi ,
I would consider the first two options as the best options in my opinion, however, sometimes the patient dislike the idea of implant then I will consider ortho extrusion, new post, core and xrown as the third option as I don’t highly recommend a bridge there, because, the adjacent teeth look like virgin teeth to me (no existing fillings/treatment).
Ara on November 26, 2016
The worst looking tooth is better than the best implant system. That’s my choice. Fight ’til the end.
Doris Ferres on October 23, 2016
If this was my tooth, I would go with option #1. So this would be my recommendation for the patient. My second recommendation would be choice #2. If patient is opposed to implant placement, my 3rd recommendation would be a Zirconium Maryland bridge with feldspathic porcelain on the inner part of the wing for proper bonding. Assuming occlusal stability has been achieved.
Manisha on September 9, 2016
Saving this tooth is not a good long term option. I would extract the tooth and plan for a graft and implant/bridge based on the the patient’s choice. Crown lengthening / orthodontic eruption will not be a good solution because we will alter the crown/root ratio (especially with the decay in the cervical third of the crown). Saving this tooth is not a good long term option for this patient.
S on September 8, 2016
Would you consider another option..short term recement with extrustion if root using ortho which will give you a ferrule as well. Once in suitable position a new post crown and correction of occlusion
Ahlam on September 8, 2016
If aethetics is a major concern of the patient and he has high lip line I would go for immediate implant with bone and soft tissue graft.
If the patient is good motivated with perfect oral hygiene I will do orthodontic crown lengthining for the root ( not surgical ) to keep the gingival outline and gingival zineth then post and core and crown will be my conservative choice
Mouhssine Alj on September 4, 2016
Hi Stephen,
First of all, thank you for sharing your experience and your knowledge.
In my opinion, I remove the remaining dark root, graft and place an immediate implant, for better
esthetic gingival results, and use à zirconium abutment.
Jordan Johnson on August 31, 2016
Recement but have a discussion with the patient that if the crown comes off again a implant will be needed. My pts seem to like having me always try the least expensive route first.
Ron Hickerson on June 26, 2016
1) I would remove decay to see how much healthy tooth I have to work with
2) I would view upper lip line in repose and full smile( it looks like tissue is thick- good biotype for any restoration, not sure about lip line from photo’s)
3) I would evaluate occlusion( looks like anterior wear patterns)
4)) I would discuss options with patient as you have outlined but add
8) thicker post/buildup/crown with minor orthodontic super eruption( or full ortho) and minor CL
If patient really wants to save tooth, is willing to accept risks and has high lip line I would choose option 8 above.
If not, I would extract/immediate implant and stage the restorative temp crown 2 months after extraction with bite guard
Kaung Myat on June 19, 2016
I’d like to choose treatment option 7 if the patient has financial concern. If not, i’ll choose option 1.
Cole on May 28, 2016
How old is the crown?
Was the patient pleased with the esthetics? If so I’d recement everything. It probably just needs a better cement
If patient doesn’t like it…
It’s a little dark under the gum there. I might add some internal bleaching first and then a new fiber post with emax crown
kinjal on May 28, 2016
I would never extract a front and would follow similar line of treatment as you have
Felipe Parra on May 28, 2016
Obviusly I take option 6 cause the x ray shows it ‘s retreat all ready due the Endo -perio and occlusion aceptable condition , an stain tesue Is not always a decay one.well done
Superna Tiwari on May 27, 2016
I would go for crown lengthening.. followed by new post core and crown
Steve S. on May 26, 2016
If the patient is not concerned about the aesthetics of the existing prosthesis and is concerned about cost it would be reasonable to recement the existing post/core and crown.
If the patient wants a better long term option then I would extract, immediate P/- with the view to placing an implant in 3 months.
Either way the occlusion/TMD issues need to be dealt with concurrently.
emilia on May 26, 2016
The last option, new post recemented with the best technique, done imediately or in the lab, cut the gingiva and let it heal with a temporary crown, make a more esthetic permanent crown, in good occlusion and discuss about the possible reduced longevity of this silution. But we have time for an implant later.
dr joe nolan on May 26, 2016
How many of you docs out there actually have a tooth just like this one? I guess zero.
I suffered badly as a kid from appalling dentistry, I own 3upper incisors with this exact scenario, the crowns and posts were done in dental school in the mid 70’s, since then I fractured one from bruxism, had a 3 unit bridge which is still flying along.
So would the implant specialists please tell me what’s wrong with me? BTW, I do place implants too. You guys are in such a hurry with the torque wrench
Dr Luca Paolo Piroddi on May 25, 2016
My opinion is that the option 6 is not a definitive solution because 1) there is no ferrule effect and 2) recementing exactly the same structure that has already failed does not solve the problem.
The option 7 would increase the lenght of the clinical crown of the upper right central incisor having a negative impact on the esthetic unless you would associate it with also an orthodontic traction.
The other options are all doable I would go for an implant (immediate or not) with graft, which is more conservative compared to a bridge in this particular case.
Thank you for the case
Dnyaneshwar Patil on May 24, 2016
My best treatment option is:-
Remove the tooth and place an immediate loading implant provided systemic condition is favourable.
Sumeet on March 18, 2016
I would provide patient with multiple options-
1. Extract, graft, provisional and then implant after 3 months.
2. Extract graft and fixed bridge.
Post and core and recementation does not look like a good option to me.
Najiya Saeed on March 2, 2016
My treatment plan would be
1- providing night guard /habit breaker considering the chipping of anteriors
2-immediate extraction with bone graft and a provisional .
3- occlusal adjustments of upper laterals and
4- implant placement after 3 months .
joe nolan on February 29, 2016
So what’s the problem with offering the least invasive tx, as in clean the crown and recement, either use the existing post or pop a new one
in and line the crown before cementing? It is always best to start with nothing, your patients will appreciate your efforts, even if the tooth is doomed….and how many years was this tooth doing okay for btw?
Just because it is supposed to fail due all the clinical metrics does not mean that it will.
If it fits and fails in a week, that’s ok. All the other excellent options can then be explored.
If there is chronic apical infection or fracture, that’s a different conversation
Arif on January 15, 2016
I would like to ask the patient before decide,what she want to do with your options. But if she is ok with all treatment plans, i prefer to do extraction, give bone graft, place denture, and 5 month after we do implant.
Marwa hakim on January 10, 2016
I will extract the tooth atraumaticaly and place an immediate implant,bone graft, and provisional abutment .
Dr G on January 8, 2016
If the patient was agreeable, I would temporarily recement after removing recurrent decay, provided margins were acceptable. Then do full records and mounting first. Given the wear facets on 21,22,23,12,13 I would need more information on his chewing pattern; to help determine Incisal edge position to permanently restore 11. Repose photo and wear on lower incisor wear pattern and existing anterior guidance pattern study will help to decide this. Grafting with implant would be a more predictable choice given the bone loss visible on periapical radiograph interproximally. The unfavourable crown:root ratio currently would caution me against putting another post/core/crown. The gingival margin is lower on the 21 than the 11, so depending on whether he shows that in smiling this may need to be altered. The question I would be asking is: How long did the existing post/core/crown last and why did it fail? If guidance was the issue then this will need to be sorted in the occlusion design or else even implant option could fail also.
Sanket on December 6, 2015
Considering the long term prognosis, I will prefer extraction followed by socket grafting and then implant
Larry Meyer on October 30, 2015
I have one today at 1:00pm with good buccal bond.
Will extract, immediate implant, and temporary crown.
Larry Meyer on October 30, 2015
Buccal bone
Norberto on October 27, 2015
1st and option with the best long term prognosis. Extraction with immediate implant and loading. Protect the gingival arquitecture with the temporary and deliver a final restoration once the gingiva and the implant is stable and oseointegrated.
Shahriar Sanati on October 27, 2015
Options you gave were basically what I would suggest too apart from a fixed bridge. I find it cruel, out of date and destructive. I only do bridges when it is a redo bridge or neighboring teeth have already crowns, are endodontically treated or need crown for any other reason.
In this particular case I would do a new post. core and crown provided that I can get ferrule without too much lengthening which will cause uneven gum line with the neighboring central.
But but but it all depends on WHO you treating. Predictability is a big factor and with the above option it might not be as predictable as , say, an implant sup[ported crown. So again it depends on the patient’s attitude and wishes.
Thanks again for sharing.
Shahriar.
CPatel on October 27, 2015
If I have my own tooth I would go for post and core crown with more removal of root filling down to apically for a short term option and possible long term plan for implant with grafting .
Also I would prefer to check my excursion movement which creating load laterally and lower teeth
incisal edges of anterior looks worn or eroded so I would consider if any traumatic occlusion.
Robert Tracogna on October 26, 2015
Looking at the PA this tooth appears to have a very tapered conical root with a large endo instrumentation prep. This would put me on guard with respect to the long term prognosis of the root and possible root fracture. This would lead me away from doing another post and core crown prep not to mention that crown lengthening would have to be done to create a long enough ferrule around this tooth. I would not want to create future structural and aesthetic problems by doing crown lengthening in this area.There seems to be some bone loss already between 11 and 21.
If I want to do an implant my next concern is the amount of buccal bone on this root. It’s hard to tell the gingival thickness over the root but the grey shading tells me that it may be thin and therefore may not be conducive to an immediate implant. I don’t want to loose any buccal bone so I may lean towards extraction and bone graft to maintain both vertical and horizontal bone mass for a future implant. Maybe too cautious but it is an unforgiving area of the mouth to restore.
The occlusion is a large part of the equation and this would have to be taken into consideration as far as the design of the final restoration.
Perry on October 25, 2015
I would consider post and core with a provisional for 6 mths to assess ability to handle any functional / bite concerns and strength. Following this I would be more confident in recommending final crown or alternatively extraction and immediate implant insertion to preserve tissues with better long term prognosis .
Angela on October 24, 2015
If it was my tooth: post and crown.
Shahriar on January 10, 2016
exactly!! most of us forget that our object is a human being while giving treatment plan options. I am sure most of the dentist in this tread will do the same as you if it was their own tooth.
Justin on September 25, 2015
i would give the patient 4 options
1. Nothing
2. Extract and denture
3. Extract and bridge
4. Extract and implant
I don’t like to give recommendations to patients as I am biased towards what I feel is optimum dentistry and don’t want them to feel pressured towards it, however, if it were my mouth I would extract and place implant 4-6 weeks post extraction/ simultaneous graft.
Sorin Muntean on September 23, 2015
I would evaluate the broken tooth itself first but I need to see what’s happening also with his anterior guidance.
Why so much flattening of incisal edges of anterior teeth? After that I can take a decision. I’m leaning more toward extraction and implant as a more permanent restoration in today dentistry but in a well functioning system.
Aarti puri on September 23, 2015
Extraction and immediate placement of implant – better long term prognosis
Josh Davies on September 21, 2015
I’m of the opinion that you should try and save natural teeth before looking for replacement restorative options. However it is the cost vs longevity that is the problem. If you think you can get 5 years out of the tooth then go for it! Remember Implants have a lifespan too 🙂
vighnesh on September 21, 2015
Would consider age of patient, ecenimucs of time and money before arriving at a decision
Roberto on September 20, 2015
If it was my tooth I would extract the tooth + inmediate Implant with provisional out of occlusion+ graft; I want to spend money in a long lasting treatment…. With high predictibility.
But if there was a chance to do orthodontic extrusion ( i think it is not the case)… I would prefer that.
Thanks.
Cam Christophers on September 20, 2015
I would prep the canal for a wider post and recement the existing crown and a fibre post . That might last 5 years and would only cost $500 with no biological cost . Depends what the patient wants . I would try to get them to wear a splint
Arif on January 15, 2016
I would like to ask her, which one preferable treatment. If she ok with all of that, than i would suggest to do extraction, bone graft, place denture and 5 months later do implant.